 , Woong Sub Koom
, Woong Sub Koom , Hong In Yoon
, Hong In Yoon , Kyung Hwan Kim
, Kyung Hwan Kim , Chan Woo Wee
, Chan Woo Wee , Jaeho Cho
, Jaeho Cho , Yong Bae Kim
, Yong Bae Kim , Ki Chang Keum
, Ki Chang Keum , Ik Jae Lee
, Ik Jae Lee
Carbon-ion radiotherapy (CIRT) offers superior dose distributions and greater biological effectiveness than conventional photon-based radiotherapy (RT). Due to its higher linear energy transfer and relative biological effectiveness, CIRT is particularly effective against radioresistant tumors and those located near critical organs. Since the first dedicated CIRT facility was established in Japan in 1994, CIRT has demonstrated remarkable efficacy against various malignancies, including head and neck tumors, skull base and upper cervical spine tumors, non-small-cell lung cancer, hepatocellular carcinoma, pancreatic cancer, prostate cancer, and bone and soft tissue sarcomas. This narrative review provides a comprehensive overview of the current status of CIRT, highlighting its clinical indications and future directions. According to clinical studies, CIRT achieves high local control rates with manageable toxicity across multiple cancer types. For instance, in head and neck tumors (e.g., adenoid cystic carcinoma and mucosal melanoma), CIRT has achieved local control rates exceeding 80%. In early-stage non-small-cell lung cancer, CIRT has resulted in local control rates over 90% with minimal toxicity. Moreover, CIRT has shown promise in treating challenging cases of hepatocellular carcinoma and pancreatic cancer, where conventional therapies are limited. Nonetheless, the global adoption of CIRT remains limited due to high costs and complexity. Future directions include conducting randomized controlled trials to establish high-level evidence, integrating new technologies such as ultrahigh-dose-rate (FLASH) therapy, and expanding CIRT facilities globally with strategic planning and cost-effectiveness analyses. If these challenges are addressed, CIRT is poised to play a transformative role in cancer treatment, improving survival rates and the quality of life.
Citations


FLASH radiotherapy (FLASH-RT) is an innovative approach that delivers ultra-high dose rates exceeding 40 Gy in less than a second, aiming to widen the therapeutic window by minimizing damage to normal tissue while maintaining tumor control. This review explores the advancements, mechanisms, and clinical applications of FLASH-RT across various radiation sources. Electrons have been predominantly used due to technical feasibility, but their limited penetration depth restricts clinical application. Protons, offering deeper tissue penetration, are considered promising for treating deep-seated tumors despite challenges in beam delivery. Preclinical studies demonstrate that FLASH-RT reduces normal tissue toxicity in the lung, brain, skin, intestine, and heart without compromising antitumor efficacy. The mechanisms underlying the FLASH effect may involve oxygen depletion leading to transient hypoxia, reduced DNA damage in normal tissues, and modulation of immune and inflammatory responses. However, these mechanisms are incompletely understood, and inconsistent results across studies highlight the need for further research. Initial clinical studies, including treatment of cutaneous lymphoma and bone metastases, indicate the feasibility and potential benefits of FLASH-RT in patients. Challenges for clinical implementation include technical issues in dosimetry accuracy at ultra-high dose rates, adaptations in treatment planning systems, beam delivery methods, and economic considerations due to specialized equipment requirements. Future directions will involve comprehensive preclinical studies to optimize irradiation parameters, large-scale clinical trials to establish standardized protocols, and technological advancements to overcome limitations. FLASH-RT holds the potential to revolutionize radiotherapy by reducing normal tissue toxicity and improving therapeutic outcomes, but significant research is required for real-world clinical applications.
Citations

 , YoungMoon Goh
, YoungMoon Goh , Jungwon Kwak
, Jungwon Kwak
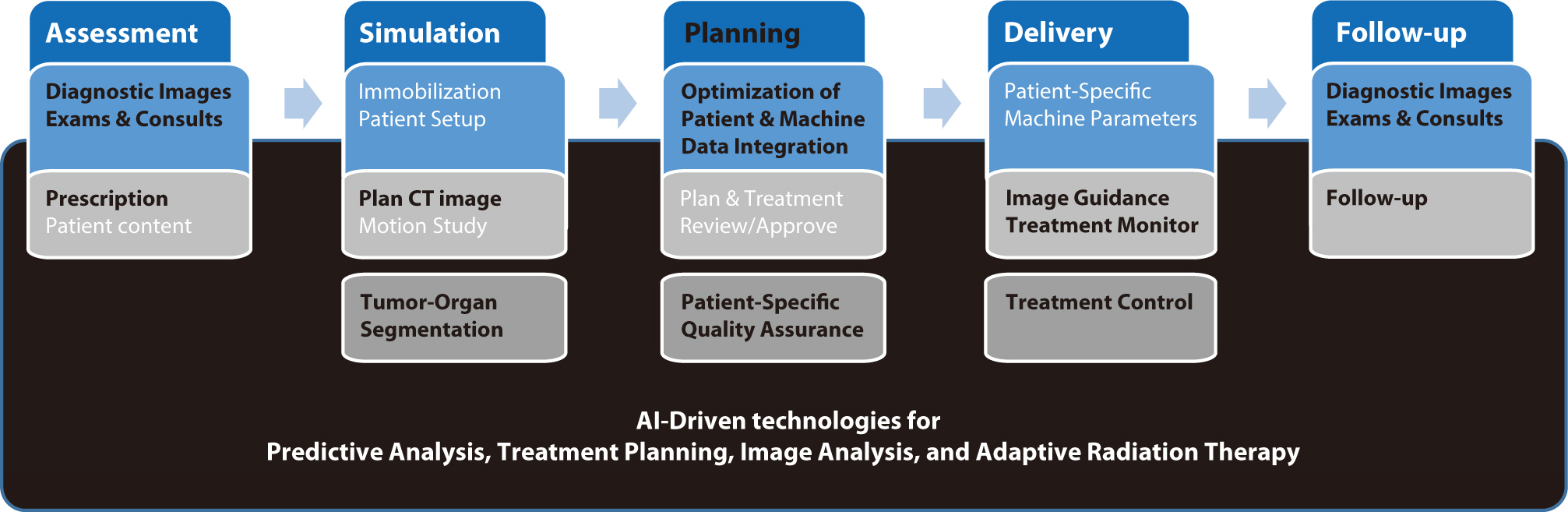
Artificial intelligence (AI) is rapidly transforming various medical fields, including radiation oncology. This review explores the integration of AI into radiation oncology, highlighting both challenges and opportunities. AI can improve the precision, efficiency, and outcomes of radiation therapy by optimizing treatment planning, enhancing image analysis, facilitating adaptive radiation therapy, and enabling predictive analytics. Through the analysis of large datasets to identify optimal treatment parameters, AI can automate complex tasks, reduce planning time, and improve accuracy. In image analysis, AI-driven techniques enhance tumor detection and segmentation by processing data from CT, MRI, and PET scans to enable precise tumor delineation. In adaptive radiation therapy, AI is beneficial because it allows real-time adjustments to treatment plans based on changes in patient anatomy and tumor size, thereby improving treatment accuracy and effectiveness. Predictive analytics using historical patient data can predict treatment outcomes and potential complications, guiding clinical decision-making and enabling more personalized treatment strategies. Challenges to AI adoption in radiation oncology include ensuring data quality and quantity, achieving interoperability and standardization, addressing regulatory and ethical considerations, and overcoming resistance to clinical implementation. Collaboration among researchers, clinicians, data scientists, and industry stakeholders is crucial to overcoming these obstacles. By addressing these challenges, AI can drive advancements in radiation therapy, improving patient care and operational efficiencies. This review presents an overview of the current state of AI integration in radiation oncology and insights into future directions for research and clinical practice.
Citations


Preoperative chemoradiotherapy (pCRT) followed by total mesorectal excision is the accepted standard treatment for patients with locally advanced rectal cancer. The purpose of pCRT is to prevent the spread of viable tumor cells within the local area during surgical procedures. Additionally, pCRT can facilitate the resection of locally advanced tumors that are otherwise challenging to remove, thereby enabling a radical resection. Although a pathologic complete response is observed in fewer than 20% of patients, the reasons for the variability in tumor response to pCRT are not fully understood. Several techniques have been researched with the aim of improving the tumor response to pCRT. These techniques include intensifying or combining chemotherapy, either simultaneously or sequentially, increasing radiation dose, modifying radiation mode or schedule, adjusting the interval between radiation and surgery, and incorporating multiple agents to increase the efficacy of pCRT. This review discusses various strategies that may improve tumor response outcomes following pCRT.
Brain metastases are a leading cause of morbidity and mortality for patients with systemic cancer and are among the most common intracranial tumors in adults. Its incidence increases as cancer therapies improve, and patients live longer, providing new challenges to the multidisciplinary teams that manage these patients. The contemporary neurosurgical treatment of intracranial metastases has become gradually more complex as the available therapeutic options increase. For the past 50 years, whole brain radiotherapy and systemic corticosteroids have been considered as the standard of care for patients with brain metastases. However, in recent years, stereotactic radiosurgery is spotlighted as an alternative therapeutic modality for these patients because of its relatively short, convenient, and non-invasive treatment course. Stereotactic radiosurgery is a radiation therapy technique in which multiple focused radiation beams intersect over a target, which results in the delivery of highly conformal, high-dose of radiation to the target and minimal radiation to surrounding normal parenchyma. The purpose of this review is to provide an overview of stereotactic radiosurgery as a treatment modality for patients with brain metastases.
Citations

 , Soo Mee Lim
, Soo Mee Lim , Myungsoo Kim
, Myungsoo Kim , Hyunsuk Suh
, Hyunsuk Suh
Radiation therapy has multiple roles in the treatment of meningioma although surgery remains the primary treatment of choice. In this retrospective study, we report the results of radiation therapy for meningioma as definitive, postoperative or salvage therapies.
Seventeen patients diagnosed with meningioma were treated with radiation therapy in our institute from May 2000 to October 2009. Radiation therapies were performed as definitive therapies in 8 patients, as postoperative therapies in 5 and as salvage therapies in 4. Nine patients received stereotactic radiosurgery (SRS), 2 patients fractionated stereotactic radiotherapy (FSRT), and 5 patients 3-dimensional conformal radiotherapy (3DCRT). Radiation dose were 12 to 20 Gy for SRS, 36 Gy in 9 fractions for FSRT and 50.4 Gy in 28 fractions for 3DCRT. Follow-up imaging study of computed tomography or magnetic resonance imaging was performed at 6 to 12 months intervals and neurologic exam was performed with an interval less than 6 months.
The median follow-up duration was 38 months (range, 12 to 85 months). Tumor progression after radiation therapy developed in one patient. The reduction of tumor volume measured on follow-up images were more than 20% in 4 patients and minimal change of tumor volume less than 20% were observed in 12 patients. Peritumoral edema developed in 4 patients and disappeared without any treatment. One patient had radiation necrosis.
Our experience is consistent with the current understanding that radiotherapy is as an effective and safe treatment modality for meningiomas when the tumor cannot be resected completely or when recurred after surgery.

