Department of Pediatrics, Ewha Womans University School of Medicine, Seoul, Korea.
Copyright © 2015, The Ewha Medical Journal
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
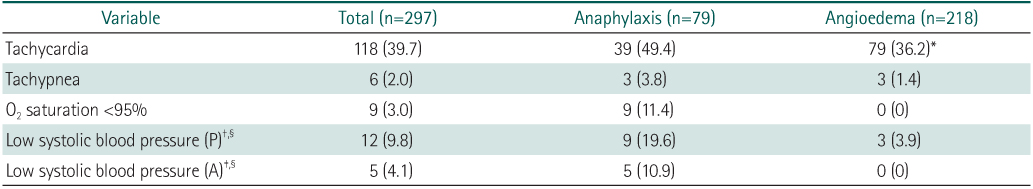
Values are presented as number (%).
*P<0.05. †According to normal vital sign from Nelson Textbook of Pediatrics. ‡According to the Clinical Criteria for the Diagnosis of Anaphylaxis. §Total (n=122), anaphylaxis (n=46), angioedema (n=76).

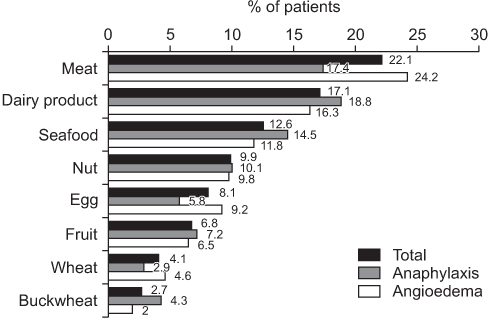
Values are presented as number (%).
*P<0.05.
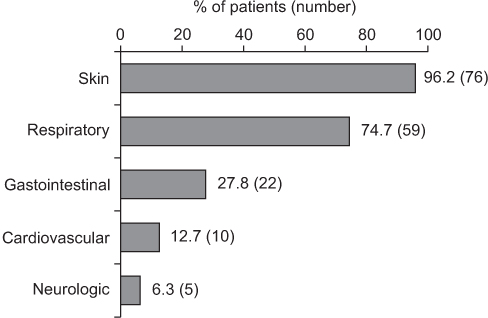
Values are presented as number (%).
*P<0.05. †According to normal vital sign from Nelson Textbook of Pediatrics. ‡According to the Clinical Criteria for the Diagnosis of Anaphylaxis. §Total (n=122), anaphylaxis (n=46), angioedema (n=76).
Values are presented as number (%).
*P<0.05.
Values are presented as number (%). *P<0.05.
Values are presented as number (%). *P<0.05. †According to normal vital sign from Nelson Textbook of Pediatrics. ‡According to the Clinical Criteria for the Diagnosis of Anaphylaxis. §Total (n=122), anaphylaxis (n=46), angioedema (n=76).
Values are presented as number (%). *P<0.05.