Department of Anesthesiology and Pain Medicine, Ewha Womans University College of Medicine, Seoul, Korea.
1Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea.
Copyright © 2017. Ewha Womans University School of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
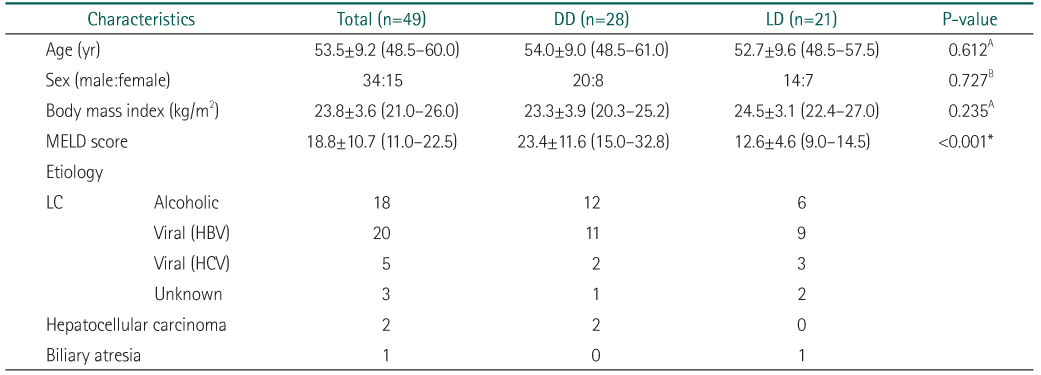
Values are presented as mean±standard deviation (interquartile range) or number.
DD, deceased donor; LD, living donor; MELD, Model for End-stage Liver Disease; LC, liver cirrhosis; HBV, hepatitis B viral; HCV, hepatitis C viral.
AIndependent t-test was done.
BChi-square test was done.
*P<0.05 (LD vs. DD).
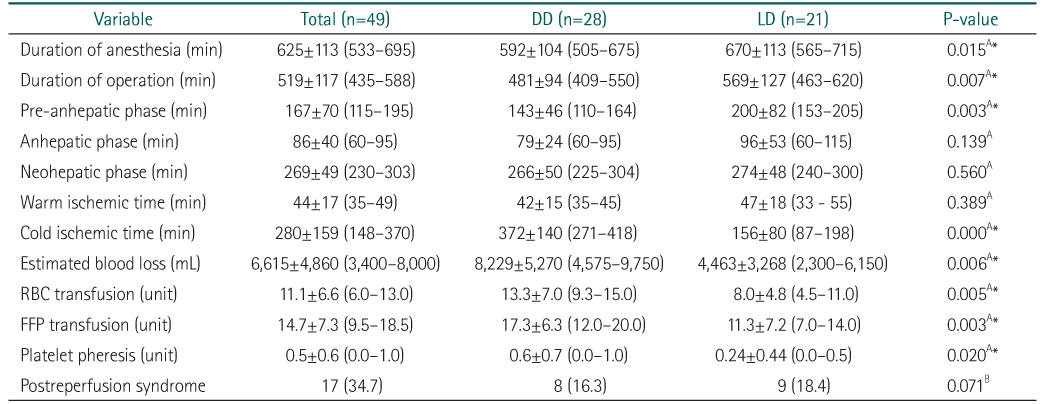
Values are presented as mean±standard deviation (interquartile range) or number (%).
DD, deceased donor; LD, living donor; RBC, red blood cell; FFP, fresh frozen plasma.
AIndependent t-test was done.
BChi-square test was done.
*P<0.05 (LD vs. DD).

Values are presented as mean±standard deviation (interquartile range) or number.
DD, deceased donor; LD, living donor; MELD, Model for End-stage Liver Disease; LC, liver cirrhosis; HBV, hepatitis B viral; HCV, hepatitis C viral.
AIndependent t-test was done.
BChi-square test was done.
*P<0.05 (LD vs. DD).
Values are presented as mean±standard deviation (interquartile range) or number (%).
DD, deceased donor; LD, living donor; RBC, red blood cell; FFP, fresh frozen plasma.
AIndependent t-test was done.
BChi-square test was done.
*P<0.05 (LD vs. DD).
Values are presented as mean±standard deviation (interquartile range). All variables analyzed by independent t-test.
DD, deceased donor; LD, living donor; ICU, intensive care unit.
*P<0.05 (LD vs. DD).
Values are presented as number of case (percentage of total patient).
CPM, central pontine myelinolysis.
Values are presented as mean±standard deviation (interquartile range) or number. DD, deceased donor; LD, living donor; MELD, Model for End-stage Liver Disease; LC, liver cirrhosis; HBV, hepatitis B viral; HCV, hepatitis C viral. AIndependent t-test was done. BChi-square test was done. *P<0.05 (LD vs. DD).
Values are presented as mean±standard deviation (interquartile range) or number (%). DD, deceased donor; LD, living donor; RBC, red blood cell; FFP, fresh frozen plasma. AIndependent t-test was done. BChi-square test was done. *P<0.05 (LD vs. DD).
Values are presented as mean±standard deviation (interquartile range). All variables analyzed by independent t-test. DD, deceased donor; LD, living donor; ICU, intensive care unit. *P<0.05 (LD vs. DD).
Values are presented as number of case (percentage of total patient). CPM, central pontine myelinolysis.