A 32-year-old female patient with chronic constipation presented with a 9-hour history of abdominal pain. She had been diagnosed with systemic lupus erythematosus (SLE) and hypertension 3 years prior to admission and received immunosuppressive drugs and steroid therapy. Her past medical history was significant for hypertension, lupus nephritis, and appendectomy. She was maintained on 5 mg prednisolone, mycophenolate, hydroxychloroquine, and fimasartan for the past 3 years.
Physical examination revealed abdominal tenderness associated with generalized rigidity and rebound tenderness; the patient also developed high fever with tachycardia and tachypnea; however, she was normotensive (38.7℃, 101/56 mmHg, 115/min, and 20 breaths/min, respectively). Blood test results showed leukocytosis (15.54×1,000/
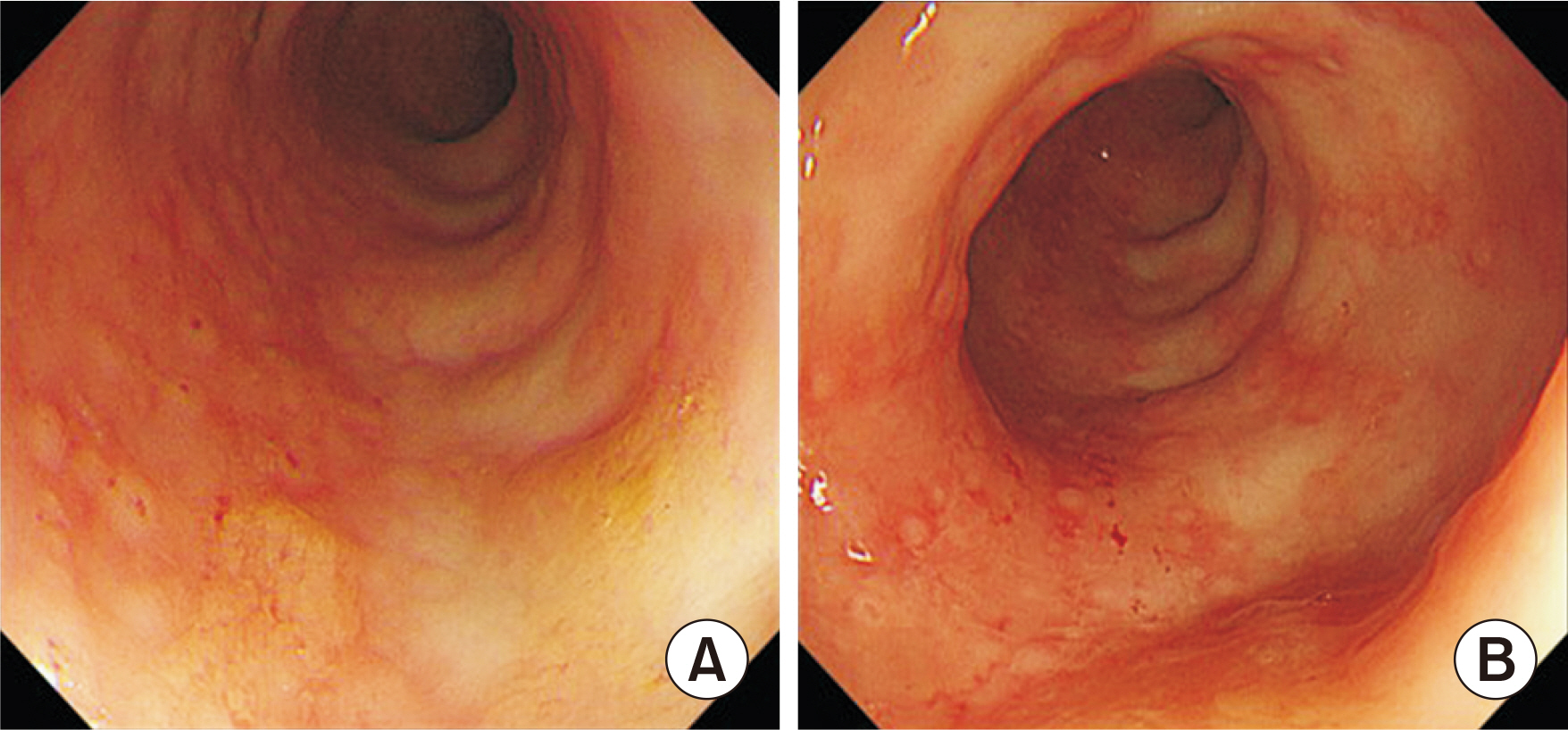
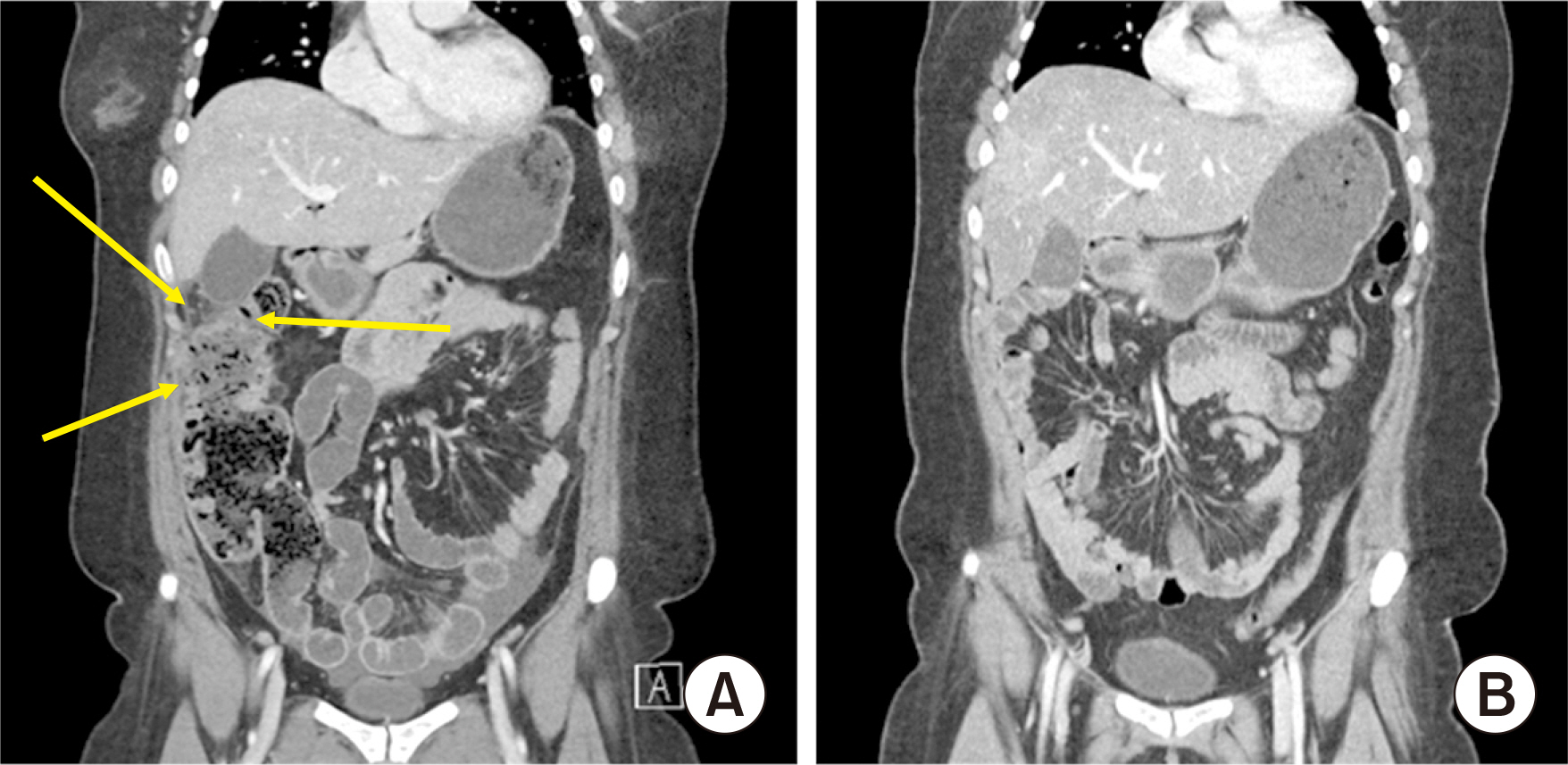
μL), elevated levels of C-reactive protein (2.09 mg/dL), and high pro-calcitonin levels of 1.04 ng/mL. Simple abdominal X-ray showed non-specific finding (
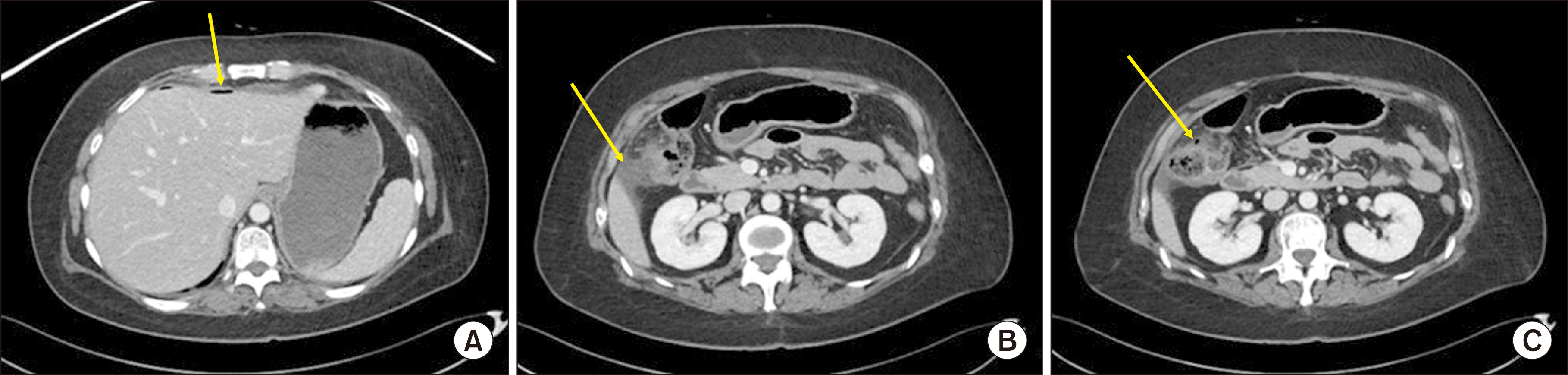
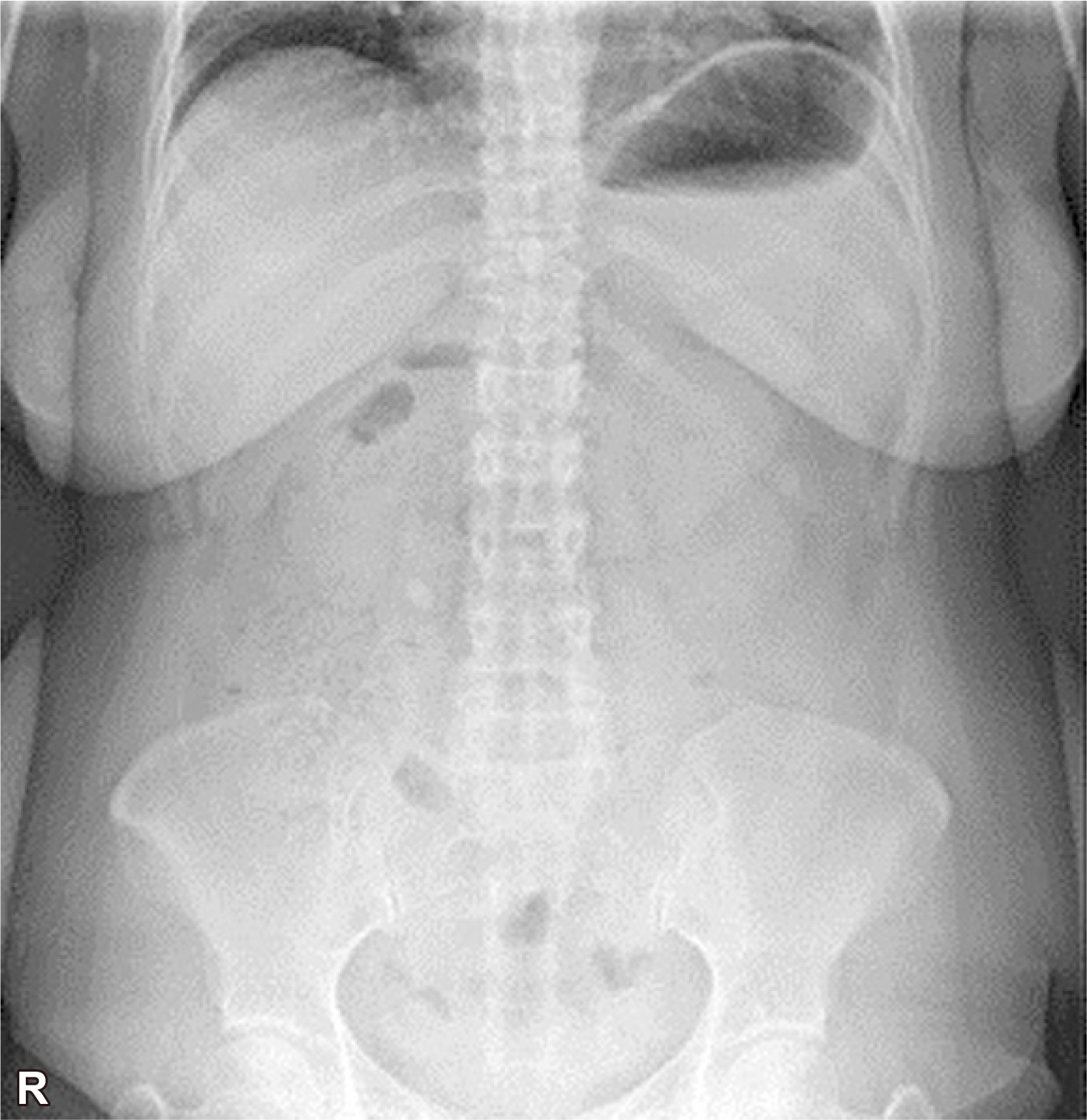
Fig. 1). Urgent abdominal CT scan revealed pneumoperitoneum in the perihepatic area and pericolic infiltration in the ascending colon with wall thickening (
Fig. 2).
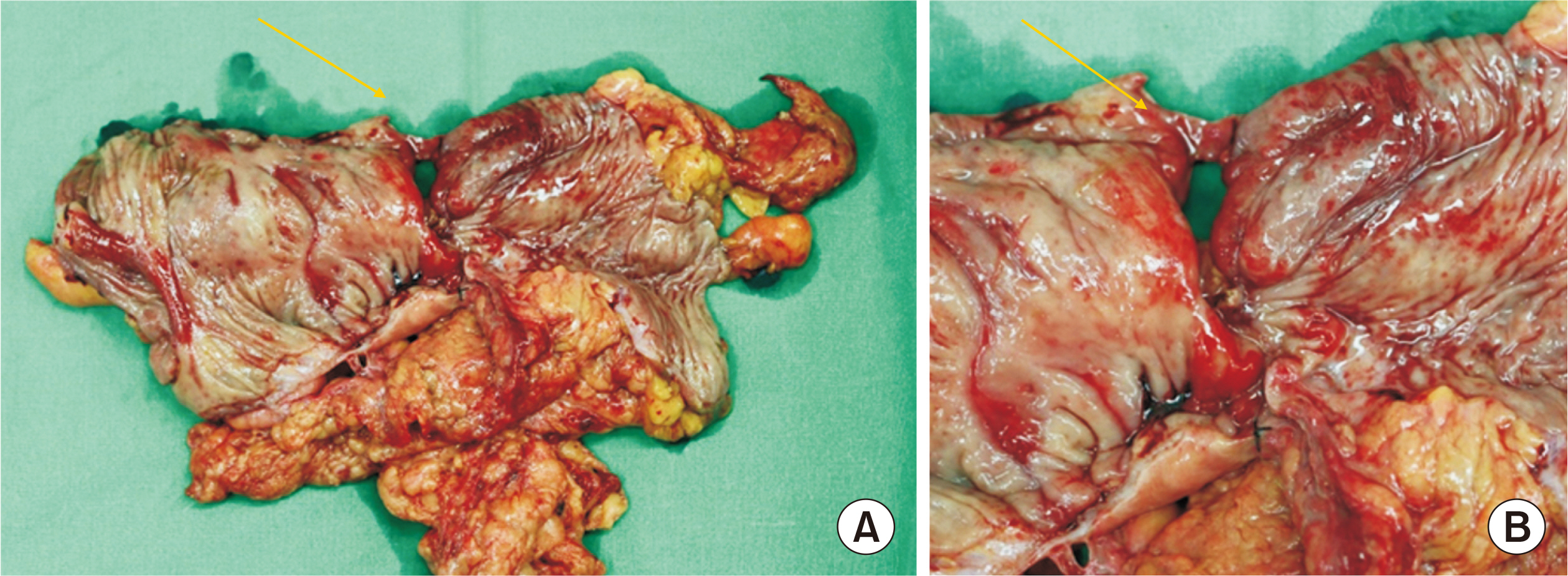
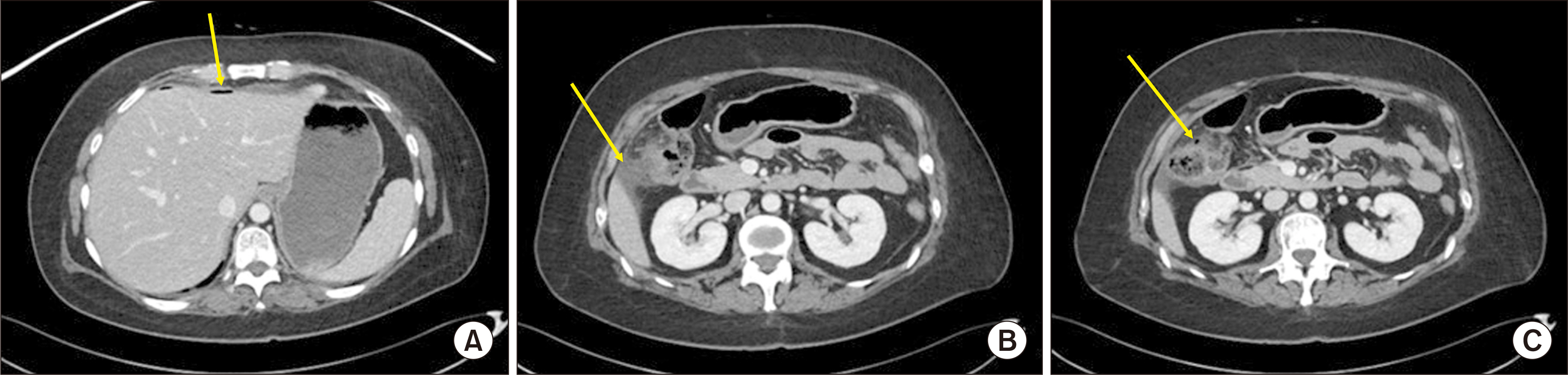
She underwent emergent laparotomy with right hemicolectomy and ileostomy; concurrently, on-table lavage was performed due to incipient diffuse purulent peritonitis. Macroscopic examination of the resected specimen revealed colonic ulceration with a perforation approximately 1 cm in size in the anterior wall of the ascending colon (
Fig. 3). Histological examination of the specimen revealed it to be an acute serositis with perforation and mucosal ischemic necrosis and submucosal and subserosal congestion.
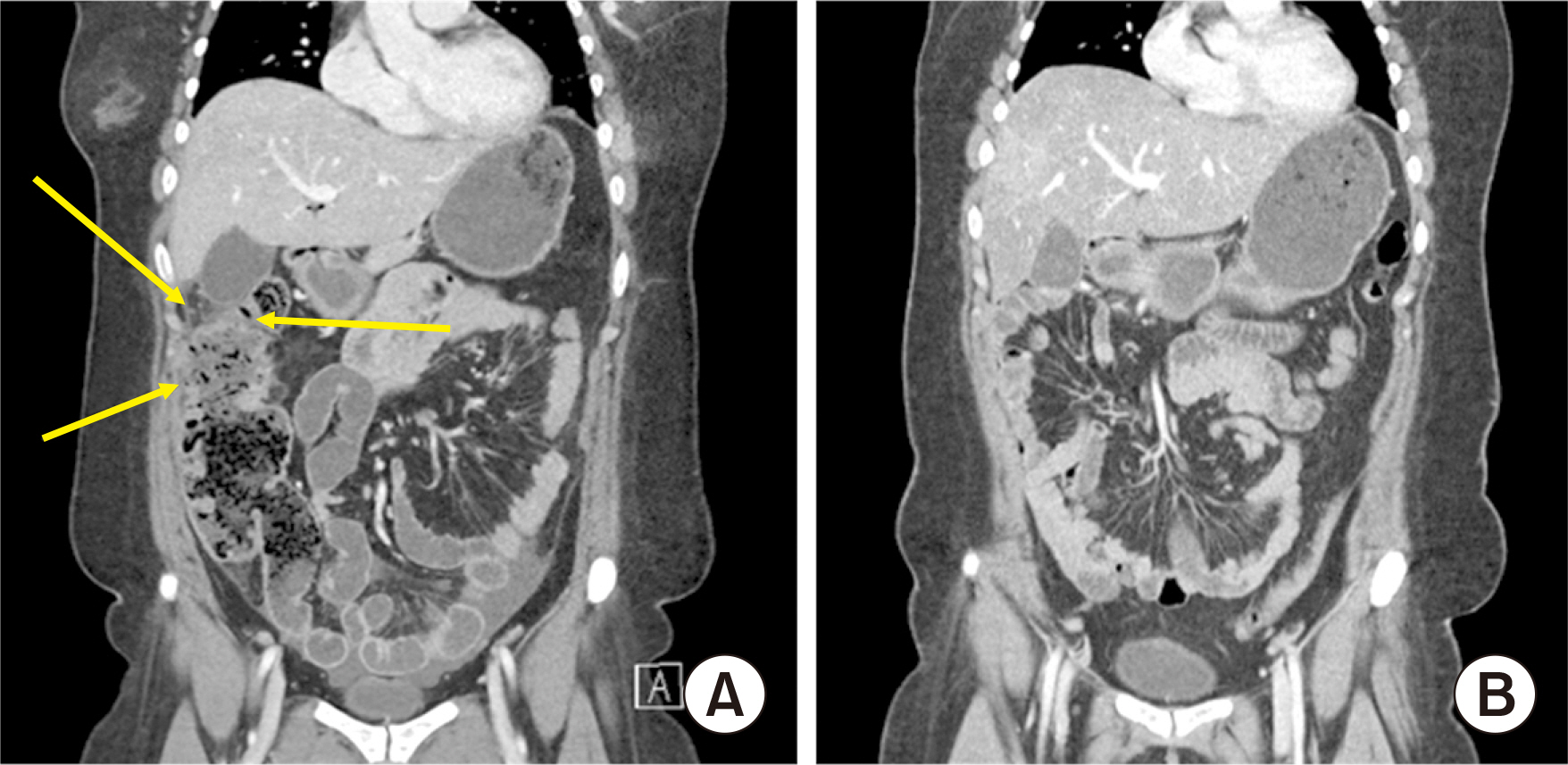
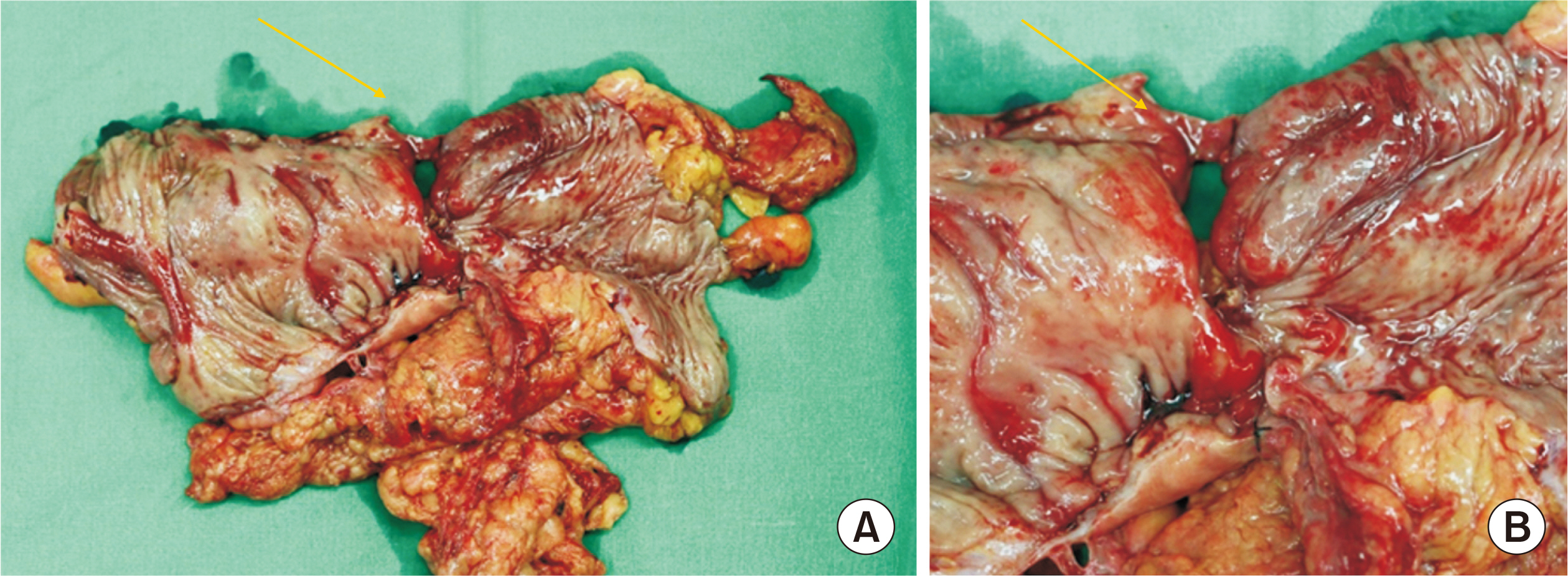
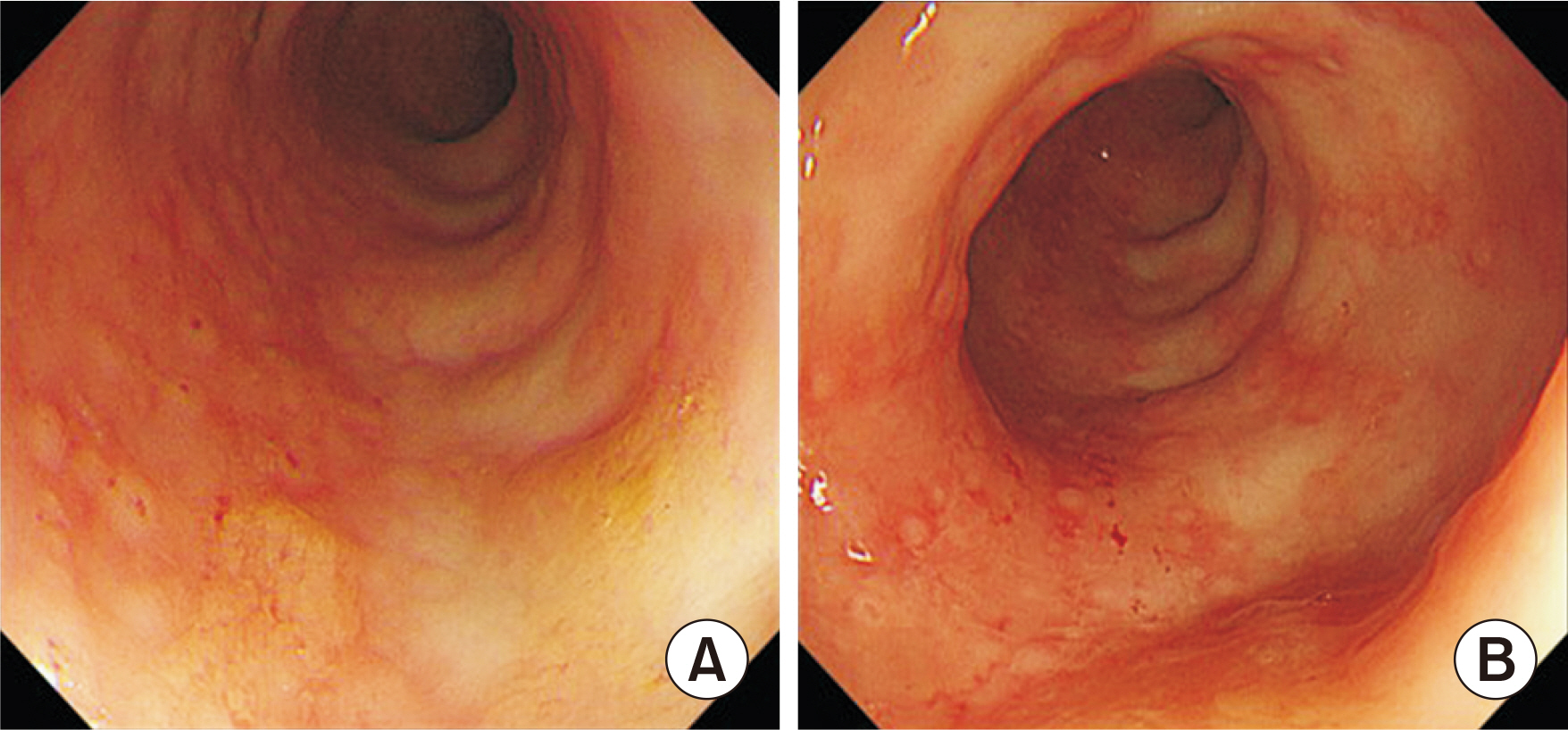
She was discharged on the 11th postoperative day without any complications. After 3 months, she underwent follow-up abdominal CT and colonoscopy (
Figs. 4,
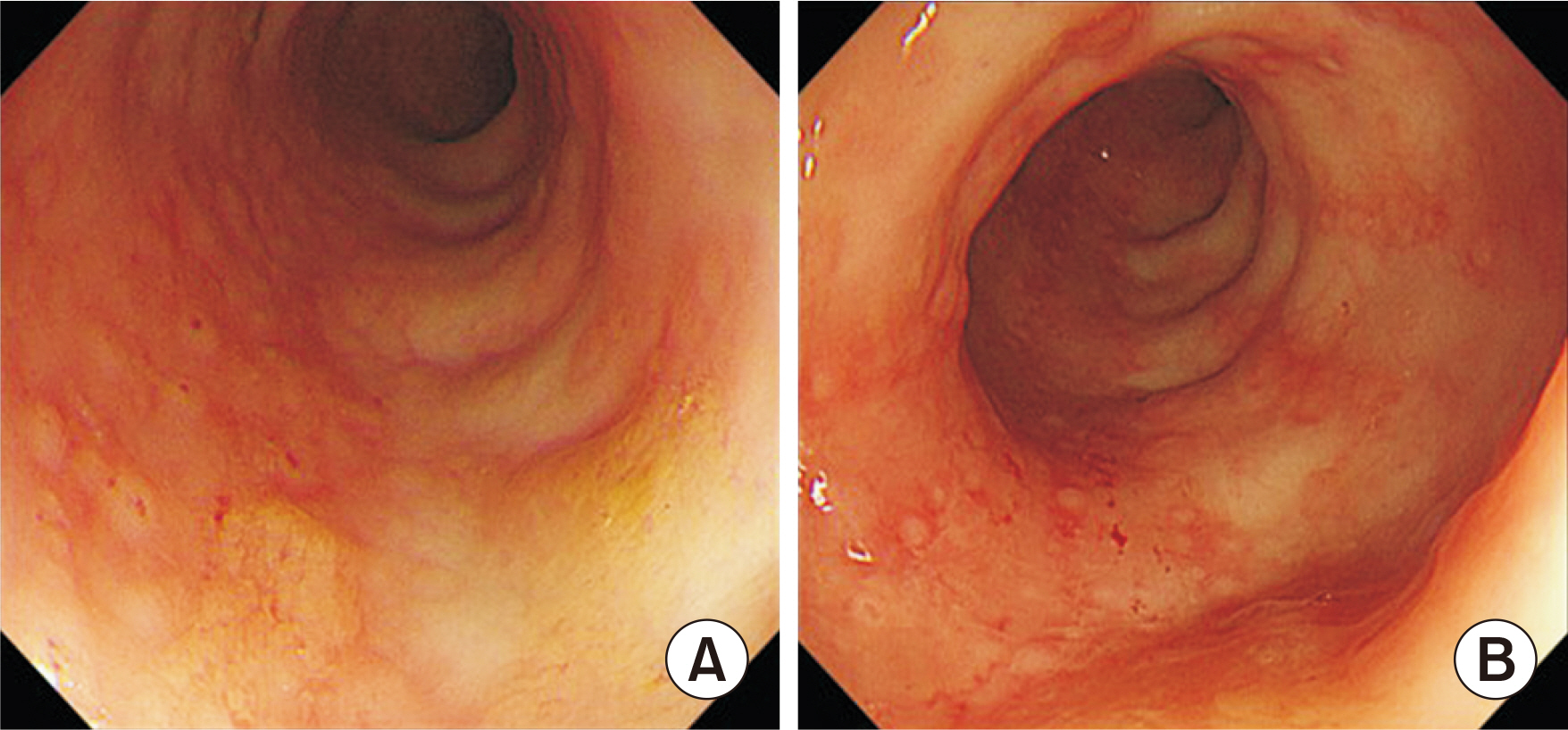
5). As there were no abnormal findings other than hyperemic mucosal change and colitis (
Fig. 5), she underwent ileostomy repair and was discharged without any complications. In this case, perforation to the necrosed portion of the colon due to long-term use of corticosteroids and immunosuppressive agents was clinically suspected.
SLE is an autoimmune inflammatory disease that results in widespread inflammation and tissue damage in the affected organs. Multiple gastrointestinal complications of SLE have been reported [
1], and the severity of lesions may be influenced by SLE activity as well as the dose and duration of steroid therapy.
Based on previous studies involving SLE patients, bowel perforation occurs occasionally for several reasons, one reason being lupus mesenteric vasculitis, which causes thrombosis that results in infarction and subsequent perforation of the bowel wall [
2]. Another proposed mechanism is steroid use in SLE, resulting in an immunocompromised state, which leads to Cytomegalovirus infection and subsequent ulceration and perforation of the bowel wall [
3]. Stercoral perforation has also been reported in several studies [
4]. Lupus enteritis can progress to intestinal necrosis and perforation.
The prognosis of SLE patients with intestinal perforation is poor; therefore, it is important to carefully take note of history of gastrointestinal symptoms, perform regular checkups, and educate the patients on possible gastrointestinal symptoms. Additionally, early diagnosis and appropriate treatment may improve the outcome in patients with SLE.
Fig. 1Simple abdominal X-ray, erect. non-specific finding. Written informed consent was obtained for publication of this case report and accompanying images.
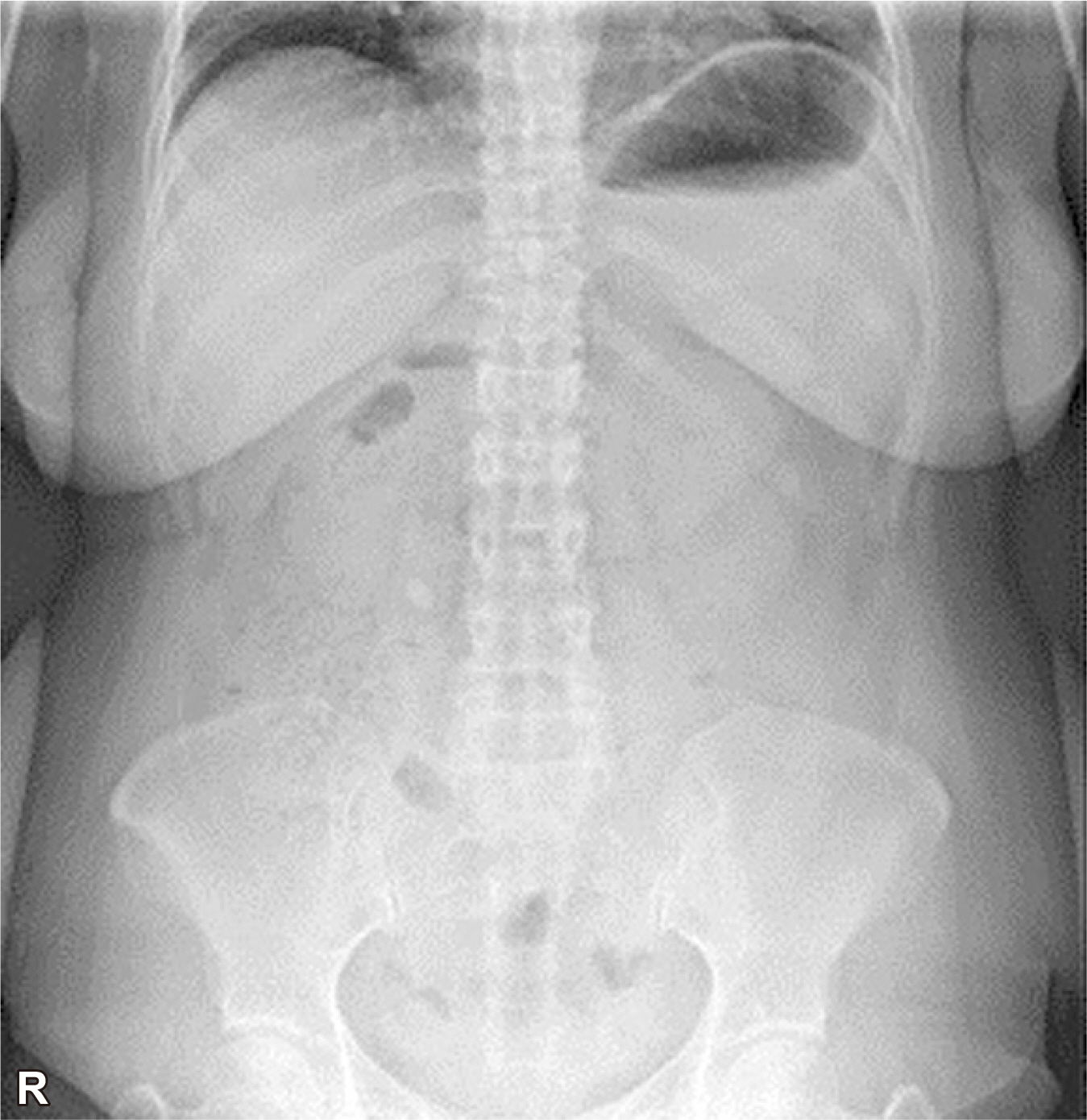
Fig. 2Preoperative abdomen CT scan. (A) Pneumoperitoneum in perihepatic area (yellow arrow). (B) The pericolic infiltration in ascending colon with wall thickening (yellow arrow). (C) Pneumoperitoneum in pericolic area (yellow arrow). Written informed consent was obtained for publication of this case report and accompanying images.
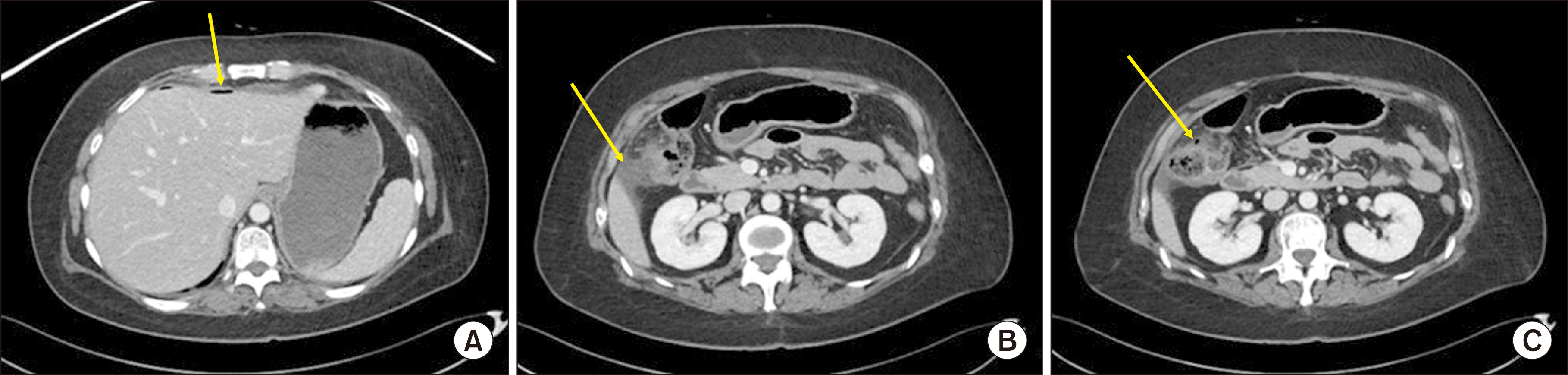
Fig. 3(A) Gross findings. A 1×2-cm-sized perforation site in colon (yellow arrow). (B) Zoom up the perforation site (yellow arrow). Written informed consent was obtained for publication of this case report and accompanying images.
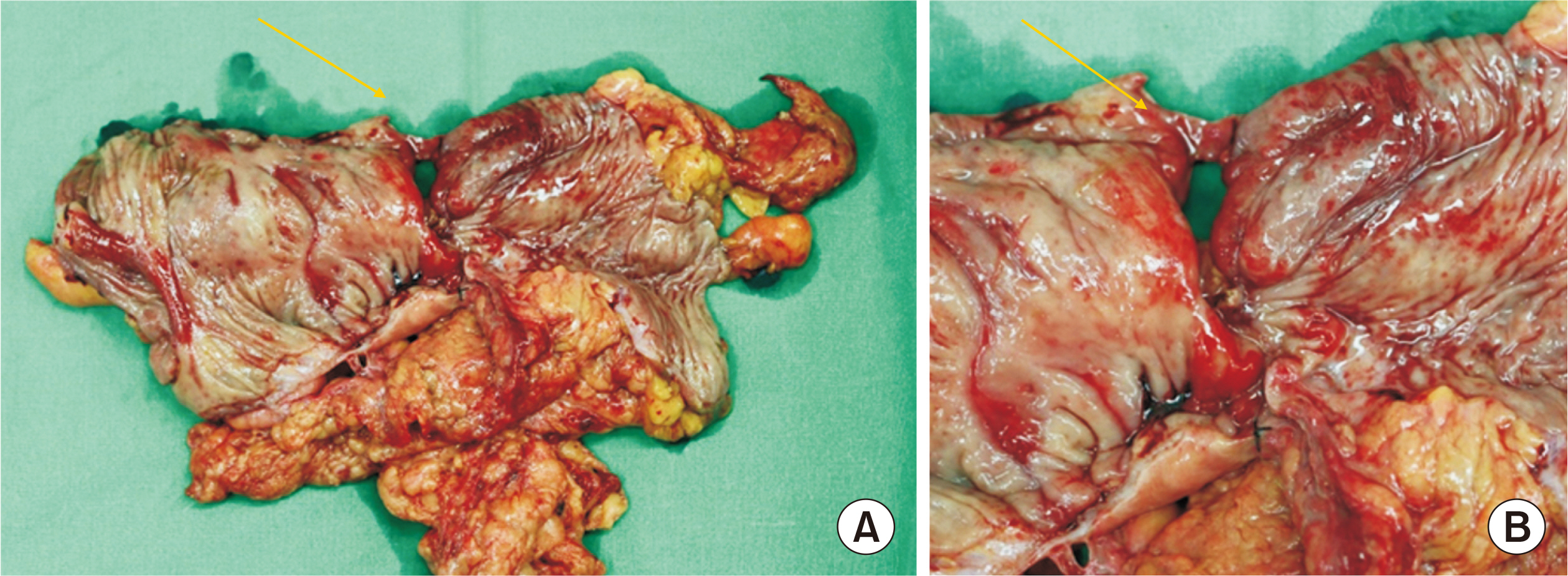
Fig. 4(A) Preoperative abdominal CT scan. Pericolic infiltration in ascending colon with pneumoperitoneum (yellow arrow). (B) Postoperative abdominal CT scan. Written informed consent was obtained for publication of this case report and accompanying images.
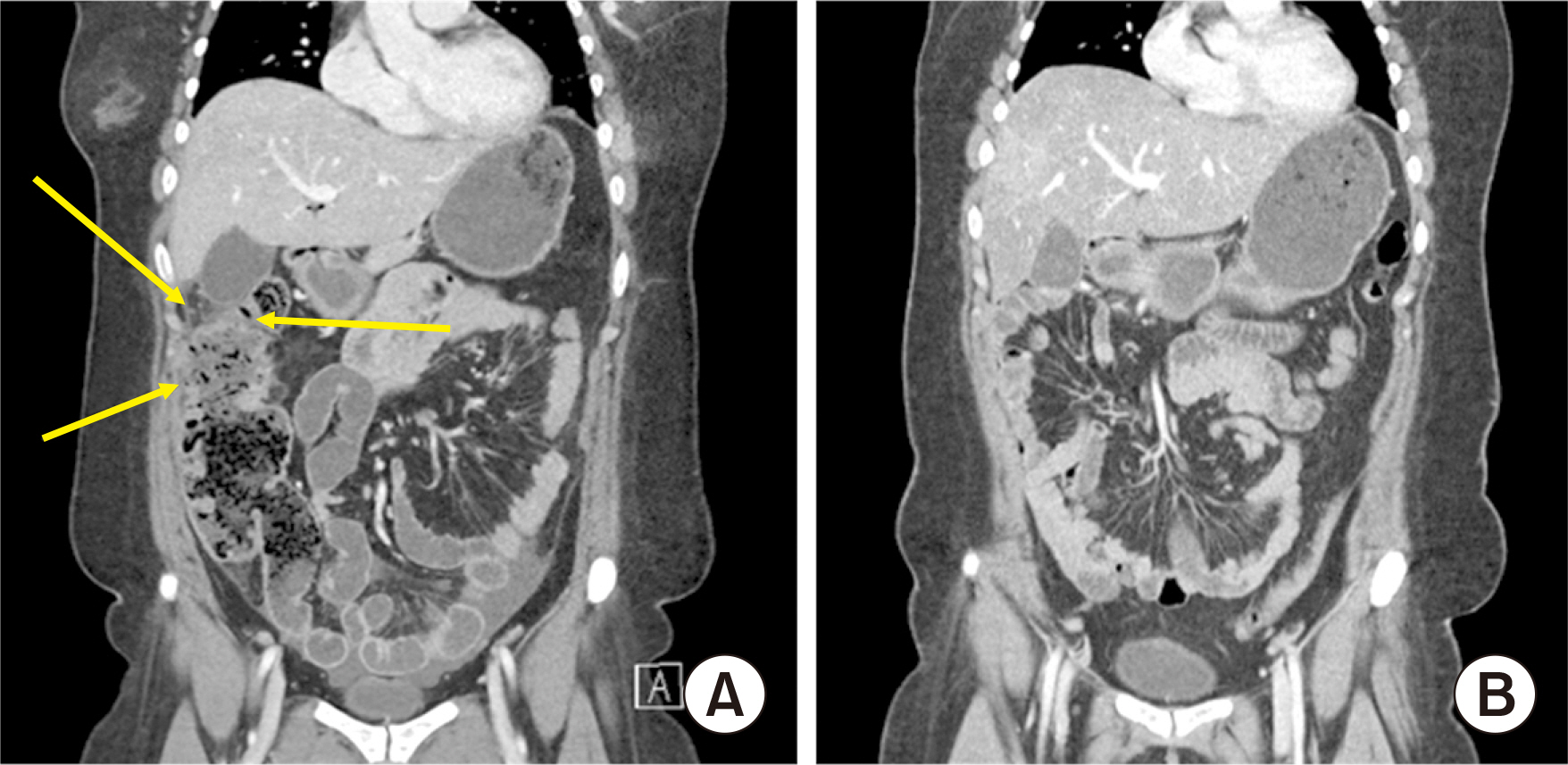
Fig. 5Colonoscopic findings. (A, B) Hyperemic mucosal change with nodular lesion. Chronic inflammation. Written informed consent was obtained for publication of this case report and accompanying images.
References
- 1. Gu Y, Zhu T, Wang Y, Xu H. 2015;Systemic lupus erythematosus with intestinal perforation: a case report. Exp Ther Med 10:1234-1238.
- 2. Huang DF, Chen WS. 2009;Images in clinical medicine. Lupus-associated intestinal vasculitis. N Engl J Med 361:e3.
- 3. ReMine SG, McIlrath DC. 1980;Bowel perforation in steroid-treated patients. Ann Surg 192:581-586.
- 4. Latif E, Musthafa S, Ahmed A, Abu Amr A. 2020;Stercoral perforation of sigmoid colon in systemic lupus erythematosus: a rare cause of peritonitis. Cureus 12:e9495.
Citations
Citations to this article as recorded by

- Hydroxychloroquine/mycophenolate/prednisolone
Reactions Weekly.2022; 1908(1): 276. CrossRef