Abstract
-
Objectives:
This study analyzed drug-induced death statistics in Korea between 2011 and
2021.
-
Methods:
Cause-of-death statistics data from Statistics Korea were examined based on
the Korean Standard Classification of Diseases and Causes of Death and the
International Statistical Classification of Diseases and Related Health
Problems, 10th revision.
-
Results:
In 2021, there were 559 drug-induced deaths, marking a 172.7% increase
compared to 2011, which recorded 205 deaths. The rate of drug-induced deaths
per 100,000 people was 1.1 in 2021, up 153.6% from 0.4 in 2011. The
mortality rate for men aged 25−34 years and women aged 35−44
years each increased fourfold from 2011 to 2021: from 0.3 to 1.2 for the
former and 0.3 to 1.3 for the latter. Of the drug-induced deaths in 2021,
75.0% (419/559) were due to intentional self-harm, and 10.4% (58/559) were
accidental. The number of deaths attributed to medical narcotics in 2021 was
169, a 5.5-fold increase from 2011. The most commonly implicated drugs in
these deaths were sedative-hypnotic drugs, benzodiazepines, and opioids.
Sedative-hypnotic drugs and benzodiazepines were frequently involved in
cases of intentional self-harm, while opioids and psychostimulants were more
often associated with accidental deaths.
-
Conclusion:
The death rate from drug-induced causes is considerably lower in Korea than
in the United States (1.1 vs. 29.2). However, the number of such deaths has
increased recently. Since these deaths occur predominantly among younger age
groups and are often the result of intentional self-harm, there is a clear
need for systematic management and the implementation of targeted
policies.
-
Keywords: Cause of death; Narcotics; Analgesics; opioid; International Classification of Diseases; Republic of Korea
Introduction
Background
Deaths caused by drugs are both preventable and avoidable. Furthermore, drug
overdose represents a significant issue that requires policy intervention, as it
can escalate into larger social problems. Recently, drug abuse has emerged as a
major global concern. According to the United States Centers for Disease Control
and Prevention, there were 106,699 drug overdose deaths in 2021, marking a sharp
increase since 2000. Notably, there has been a significant rise in deaths
attributed to opioids such as fentanyl [
1,
2]. The impact of drugs on
mortality involves both direct and indirect factors. Direct causes refer to
cases where the primary cause of death is drug-related, as classified by the
World Health Organization (WHO) in the International Standard Classification of
Diseases (ICD-10). Indirect factors involve drug use increasing the risk of
deaths from other causes, such as intentional self-harm, liver disease,
hepatitis, and heart disease. The Global Burden of Disease study reported that
drug use is responsible for approximately 114,000 indirect deaths and 350,000
direct deaths annually [
3].
This study analyzed the characteristics of drug-related deaths, aiming to inform
and support drug-related policies. Additionally, it sought to identify risk
factors associated with drug-related deaths to aid in the development of
strategies to reduce such fatalities. The report specifically focused on the
demographic characteristics, types of deaths, and the various drugs involved in
drug-induced fatalities.
Methods
Ethics statement
This study involved an analysis of public data; therefore, neither approval by
the institutional review board nor the obtainment of informed consent was
required.
Study design
This descriptive study was based on public data from Statistics Korea, and it was
described according to the STROBE Statement available from:
https://www.strobe-statement.org/.
This study analyzed microdata on cause of death statistics from Statistics Korea
spanning from 2011 to 2021 to examine the characteristics of drug-related
deaths. The cause of death statistics in Korea are compiled from death
certificates. To enhance the accuracy of determining the underlying cause of
death, Statistics Korea integrates 22 types of administrative data for each
individual. The detailed administrative data includes health insurance
information from the National Health Insurance Service, cancer registry data
from the National Cancer Center, criminal investigation records and traffic
accident investigation data from the National Police Agency, autopsy records
from the National Forensic Service, emergency records from the National
Emergency Medical Center, among others. Notably, drug-related deaths are
reliably documented, reflecting data from police investigations and autopsy
reports provided by the National Forensic Service. The ICD-10 code list for
causes of death due to drugs is provided in Supplement 1. Deaths due to drugs
were categorized by cause of death into disease, accident, intentional
self-harm, and homicide, and further analyzed by classifying the drugs involved
into opioids, sedatives, and psychotropic agents.
Bias
There was no bias in data collection and analysis.
Study size
The entire population of the Republic of Korea was included. No sample size
estimation was required.
Statistical methods
Descriptive statistics were applied to present the results of the data
analysis.
Results
Drug-induced death
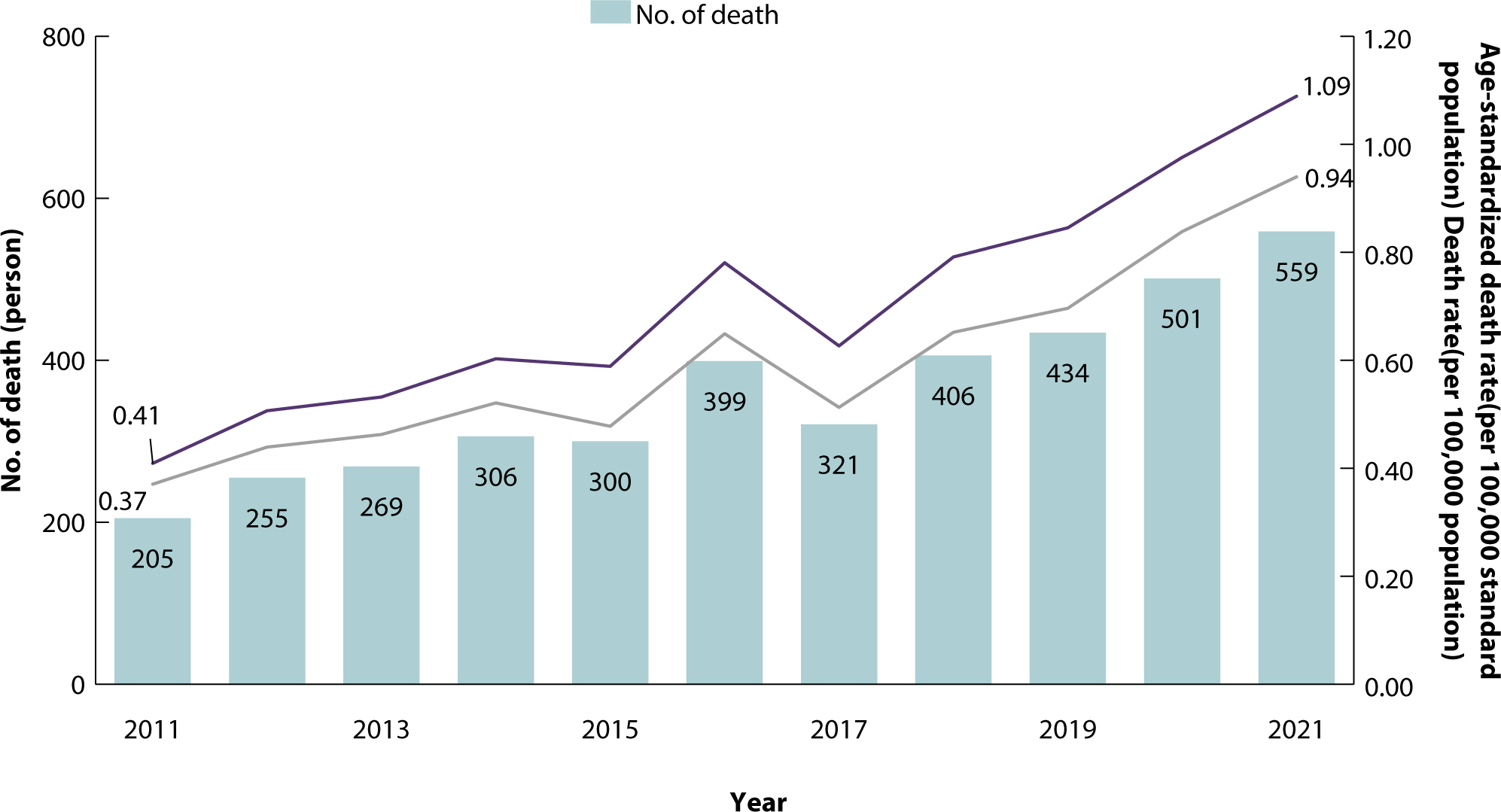
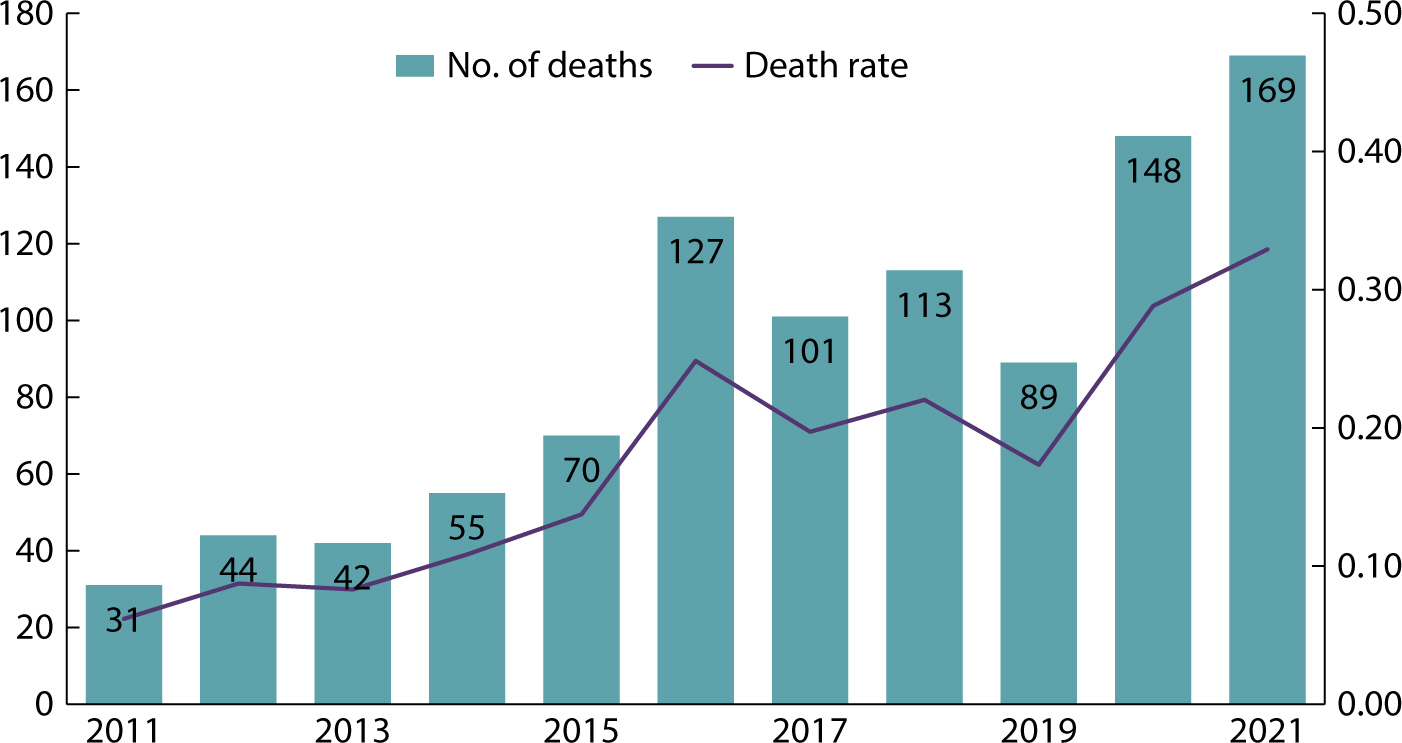
In 2021, there were 559 drug-induced deaths in Korea, marking a 172.7% increase
from the 205 deaths recorded in 2011 (
Table
1,
Fig. 1). The average number
of drug-induced deaths per day was 1.5. The mortality rate was 1.1 per 100,000
population, and the age-standardized mortality rate was 1.1 per 100,000
standardized population. Deaths due to drugs steadily increased throughout the
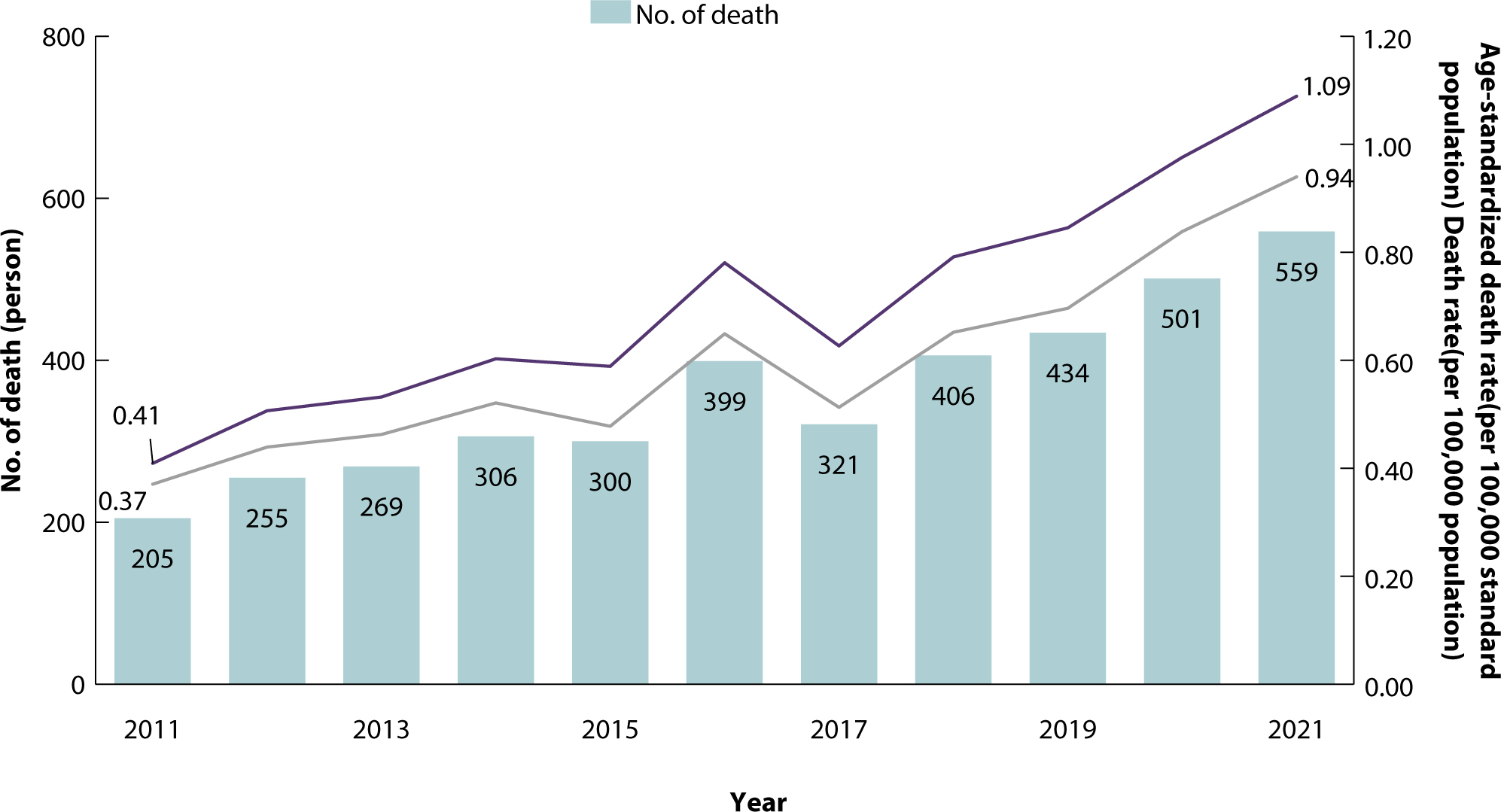
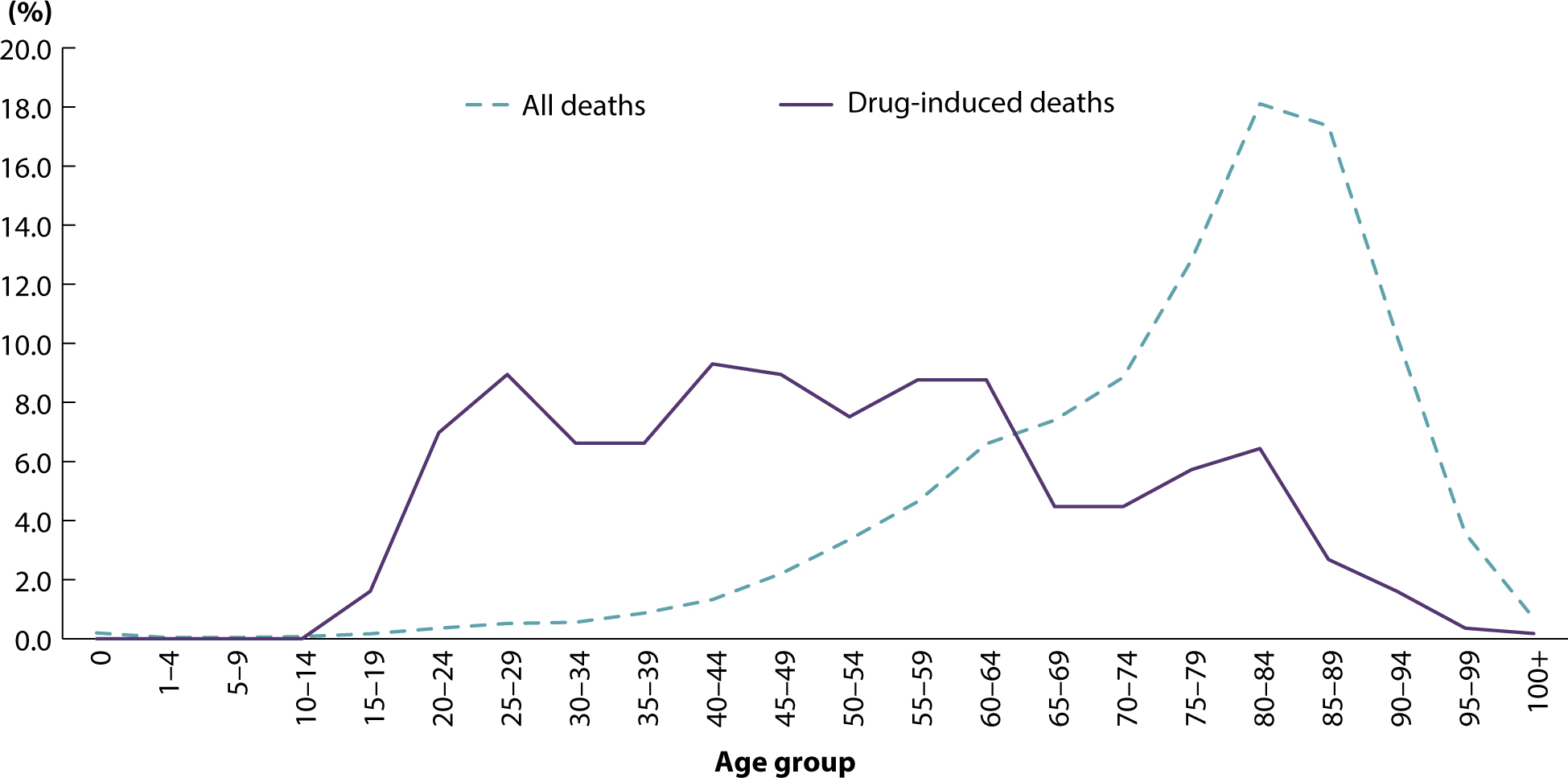
study period and predominantly occurred in relatively young age groups (
Fig. 2). While the highest percentage of all
deaths in 2021 occurred in individuals aged 80−84 (18.1%), a significant
proportion of drug-related deaths occurred in those aged 64 or younger.
Table 1.The number of drug-induced deaths, death rate, and age-standardized
death rate between 2011 and 2021
|
Year |
No. of deaths (deaths) |
Death rate
(deaths per
100,000 population) |
Age-standardized death
rate
(deaths per 100,000 standard population) |
|
2011 |
205 |
0.41 |
0.37 |
|
2012 |
255 |
0.51 |
0.44 |
|
2013 |
269 |
0.53 |
0.46 |
|
2014 |
306 |
0.60 |
0.52 |
|
2015 |
300 |
0.59 |
0.48 |
|
2016 |
399 |
0.78 |
0.65 |
|
2017 |
321 |
0.63 |
0.51 |
|
2018 |
406 |
0.79 |
0.65 |
|
2019 |
434 |
0.85 |
0.7 |
|
2020 |
501 |
0.98 |
0.84 |
|
2021 |
559 |
1.09 |
0.94 |
|
Change (absolute) |
|
|
|
|
from 2011 |
354 |
0.7 |
0.57 |
|
from 2020 |
58 |
0.1 |
0.1 |
|
Change (proportional, %) |
|
|
|
|
from 2011 |
172.7 |
166.2 |
153.6 |
|
from 2020 |
10.4 |
10.4 |
10.8 |
Fig. 1.Drug-induced deaths, death rate, and age-standardized death rate,
2011−2021 (units: people, per 100,000 people, and per 100,000
standard population).
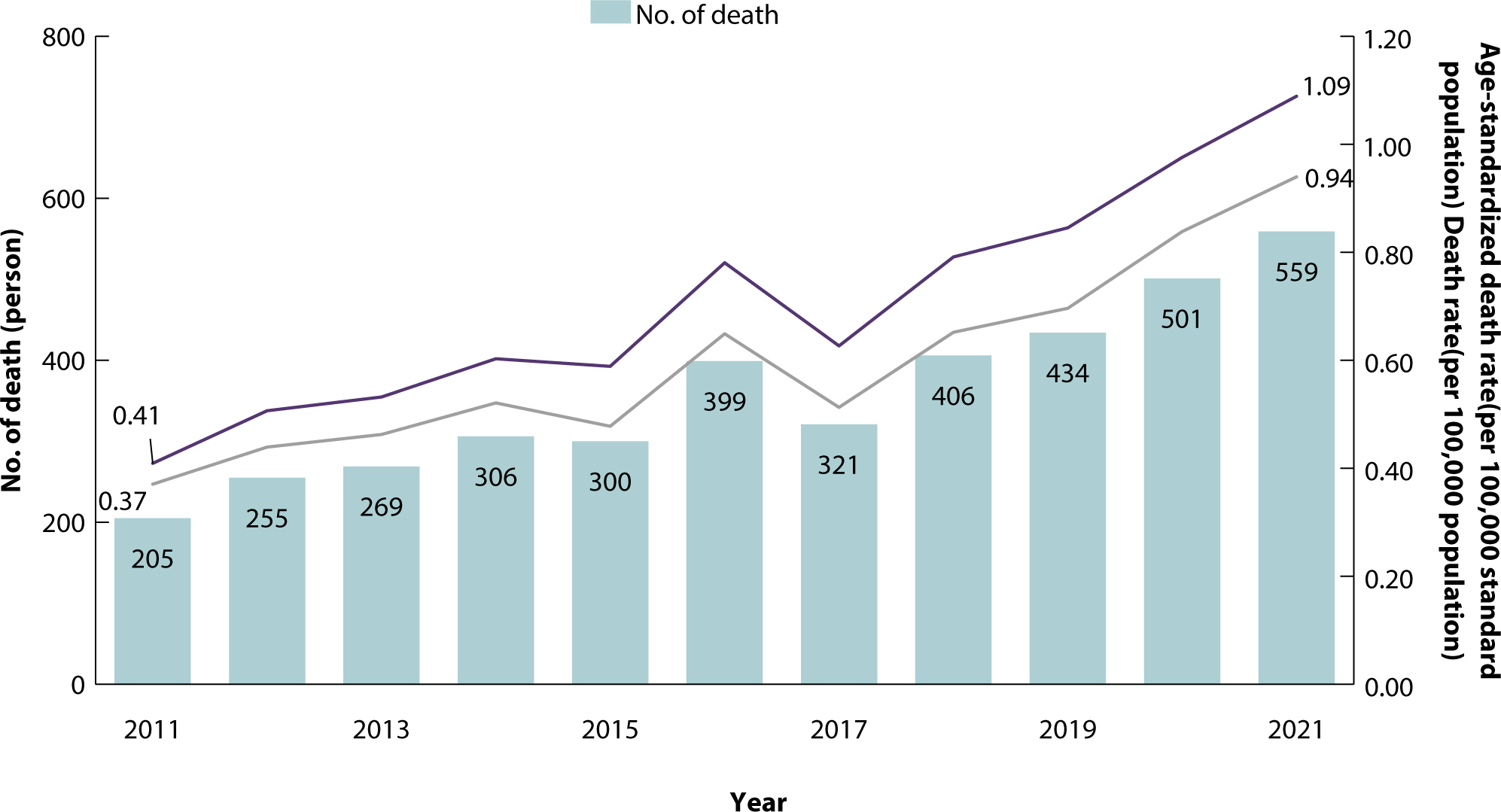
Fig. 2.Proportional age distribution for drug-induced deaths versus total
deaths, 2021.
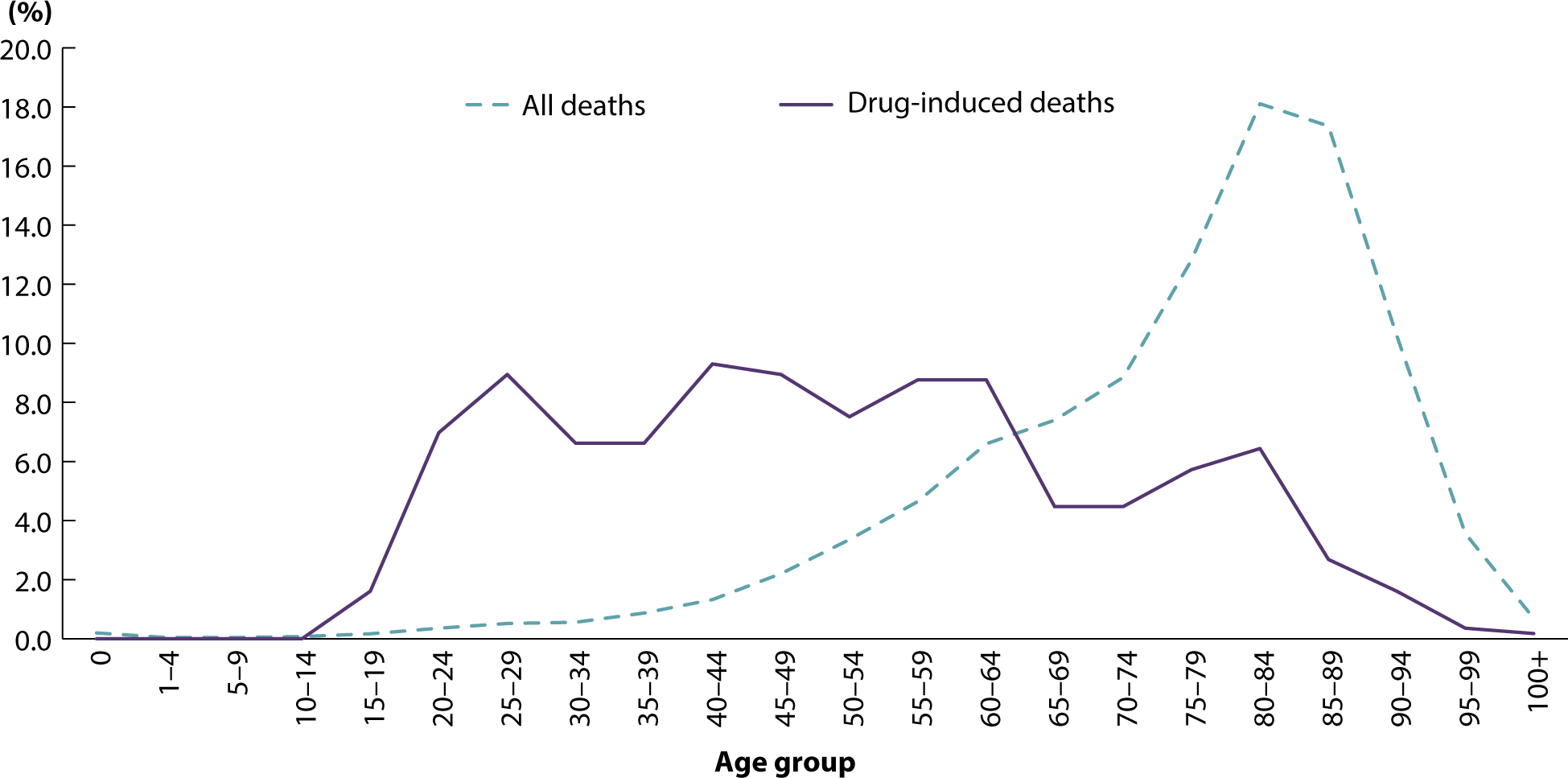
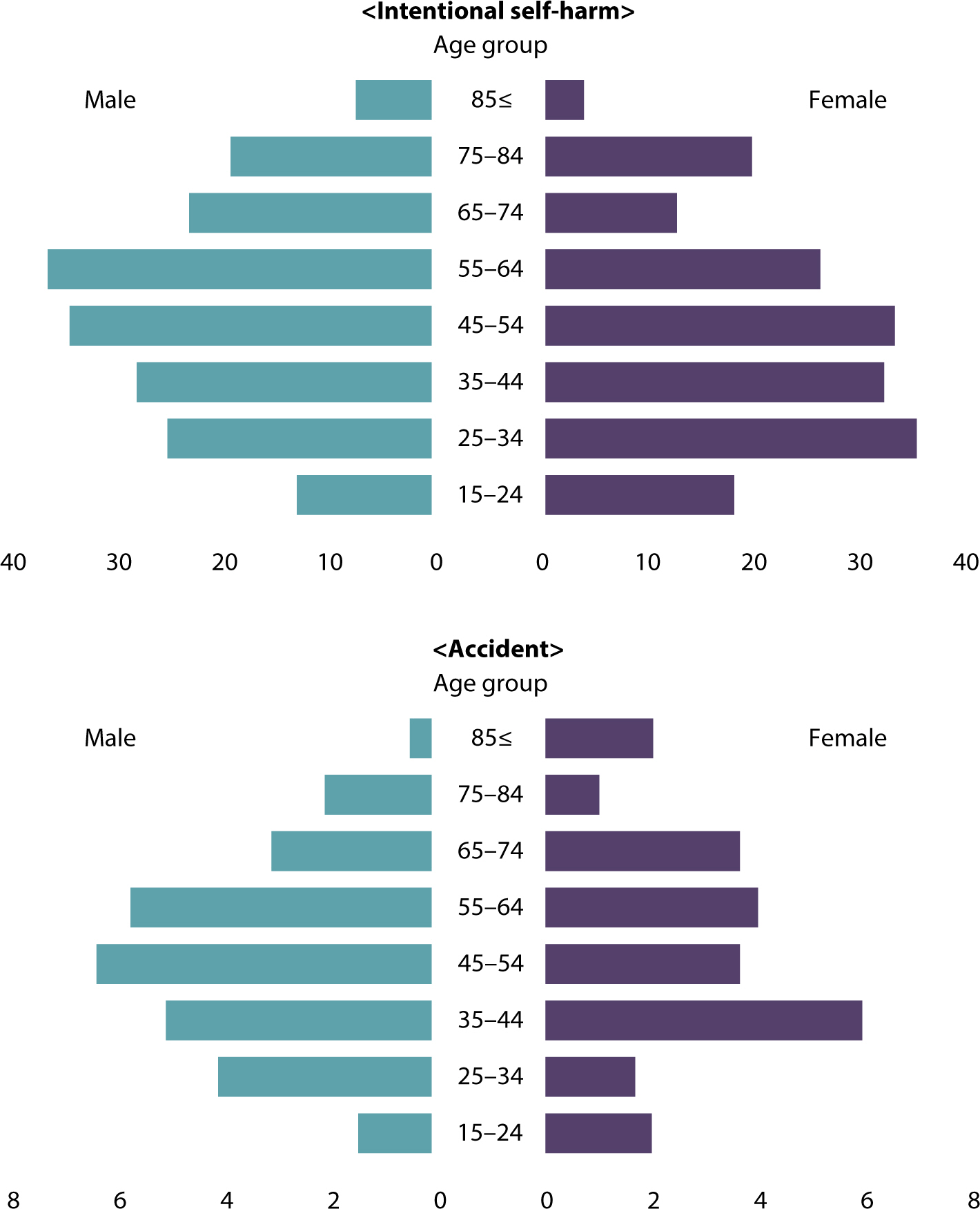
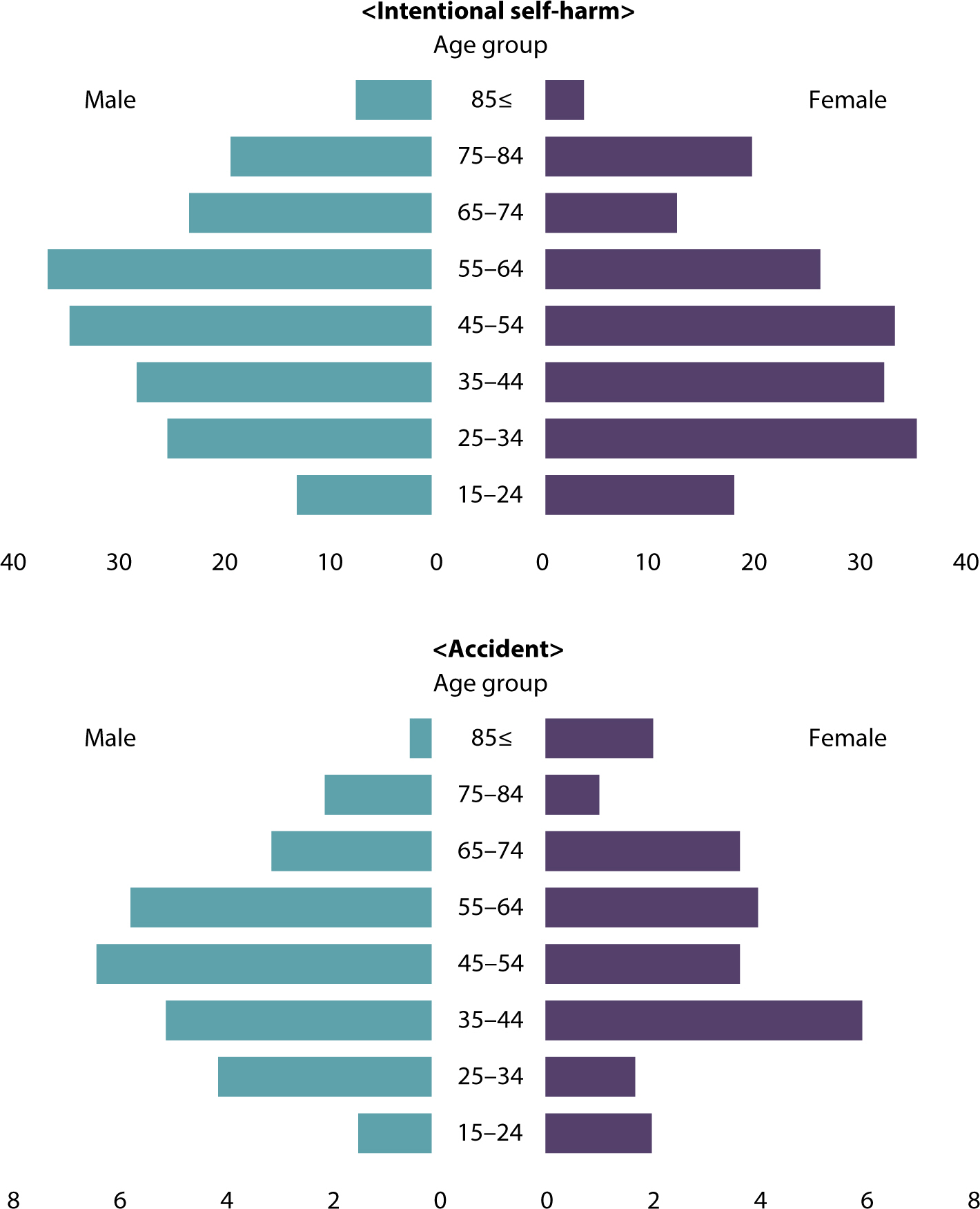
Compared to 2011, the number of deaths in 2021 increased across all age groups
for both men and women, with a notable rise in the younger demographics.
Specifically, the mortality rate for men aged 25 to 34 and for women aged 15 to
24 saw significant increases (Supplement 2). Of the deaths caused by drugs in
2021, 75.0% were intentional self-harm and 10.4% were unintended accidents. The
number of deaths attributed to intentional self-harm involving drugs has
increased since 2011. Over the past three years, the average age at death from
drug-related causes has been consistently lower for women than for men (
Fig. 3). When categorizing deaths by drug
type since 2011, the three most prevalent drugs based on their effects were
sedatives and sleeping pills, such as zolpidem and benzodiazepines; psychotropic
drugs, including antidepressants and neuroleptics; and a combination of
narcotics and psychotropic drugs, notably fentanyl (Supplement 3).
Fig. 3.Annual average number of drug-induced deaths by sex and age,
2019−2021.
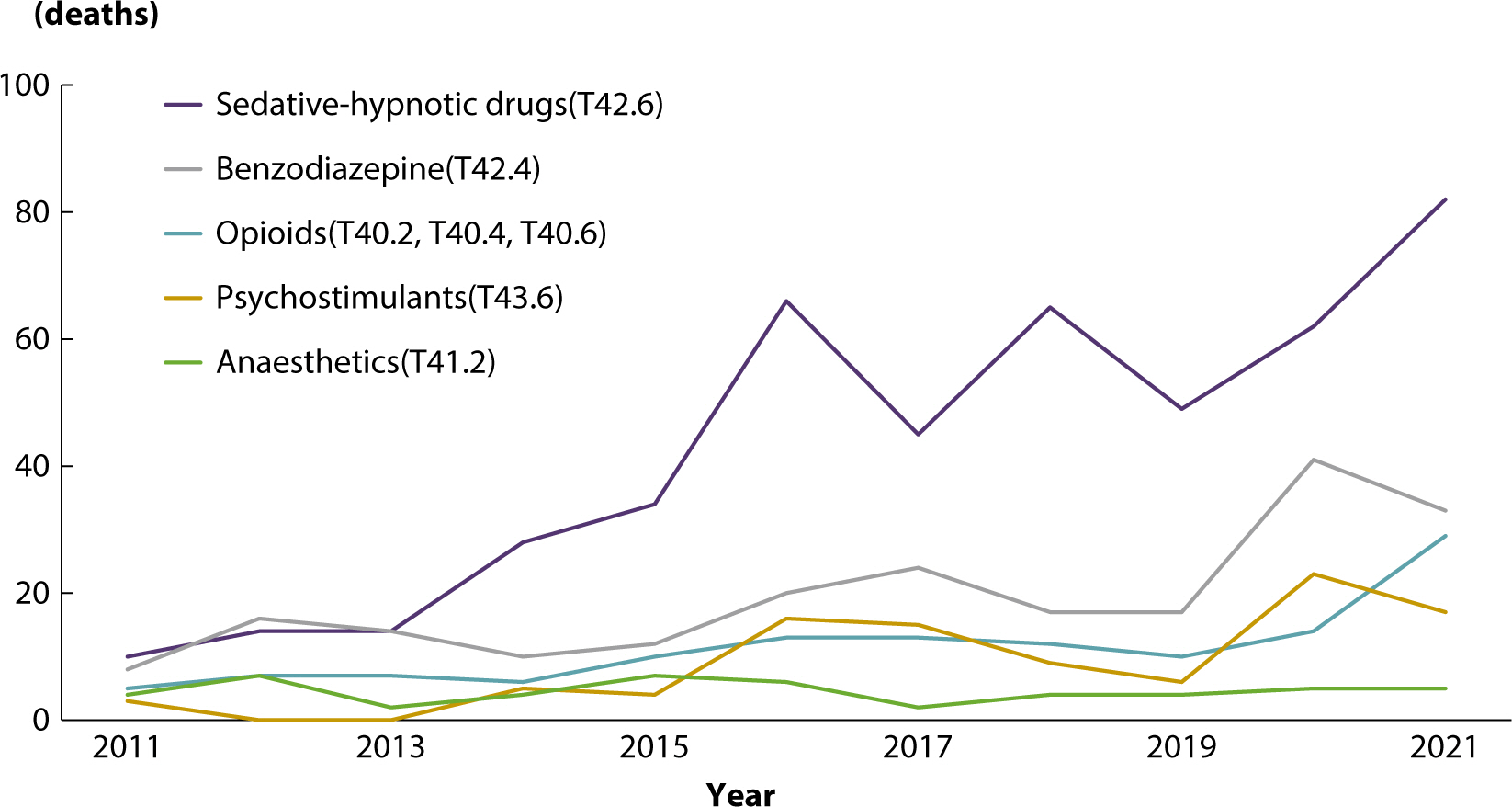
Death due to medical narcotics
To analyze deaths specifically attributed to designated medical narcotics in
Korea, narcotic drugs were categorized according to ICD-10 codes (Supplement 1).
In 2021, there were 169 deaths due to medical narcotics, representing a 5.5-fold
increase from the 31 deaths recorded in 2011. Although the number of deaths
decreased from 127 in 2016 to 89 in 2019, there has been a rapid increase for
two consecutive years (
Fig. 4). A detailed
breakdown of deaths by type of medical narcotic shows that sedative-hypnotic
drugs account for the highest number, followed by benzodiazepines and opioids.
Notably, the number of deaths associated with sedative-hypnotic drugs, such as
zolpidem, and opioids, such as fentanyl, is on the rise (
Fig. 5). Men had a higher proportion of deaths involving
psychostimulants than women, and women had a higher proportion of deaths
involving sedative-hypnotic drugs, general anesthetics, and appetite depressants
than men. An analysis of medical narcotics deaths by age between 2019 and 2021
revealed that the risk of death from narcotics varied with age. Specifically,
opioids accounted for a high proportion of deaths among individuals aged 25 to
54, benzodiazepines were involved in a large proportion of deaths among those
aged 45 to 64, sedative-hypnotic drugs predominated among those aged 55 to 74,
and deaths related to general anesthetics were most common among those aged 25
to 34 (
Table 2).
Fig. 4.Number of deaths and death rate due to medical narcotics,
2011−2021.
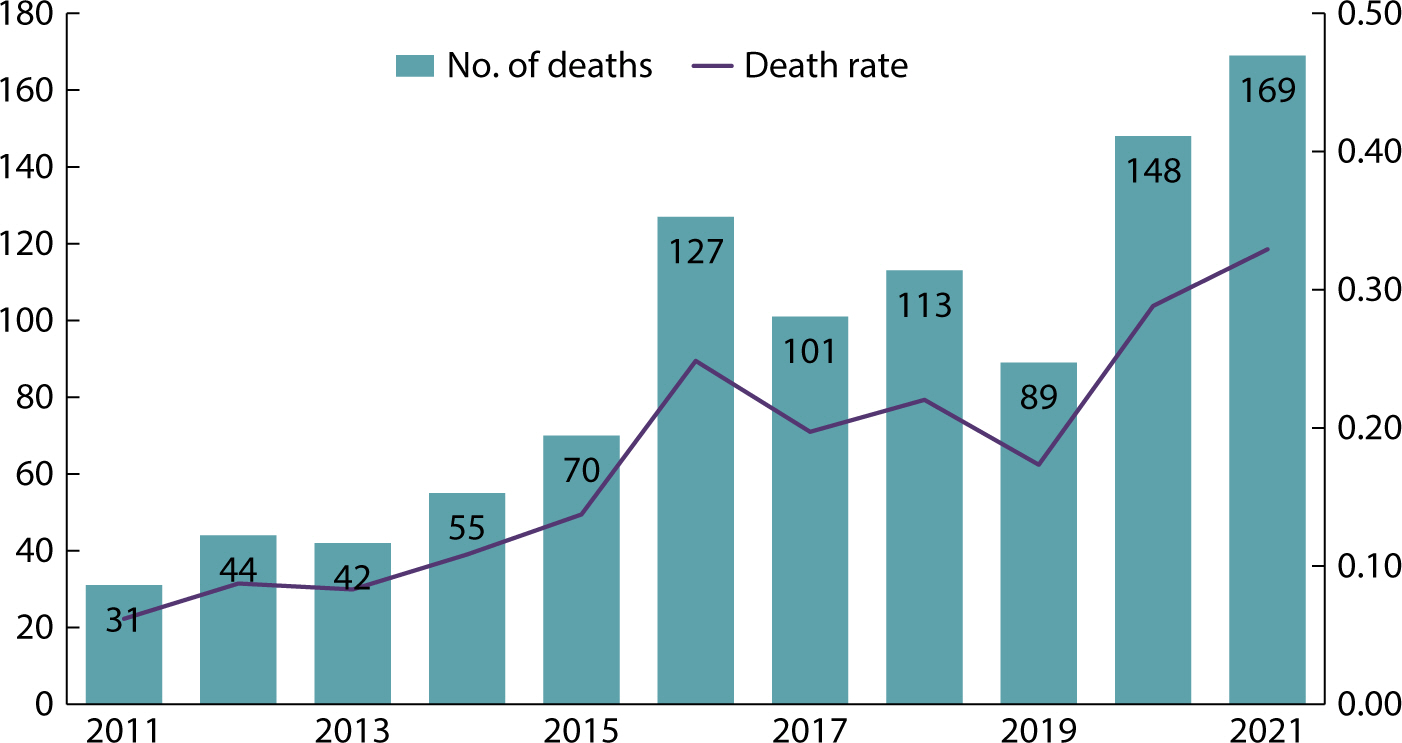
Fig. 5.Number of deaths due to medical narcotics, 2011−2021.
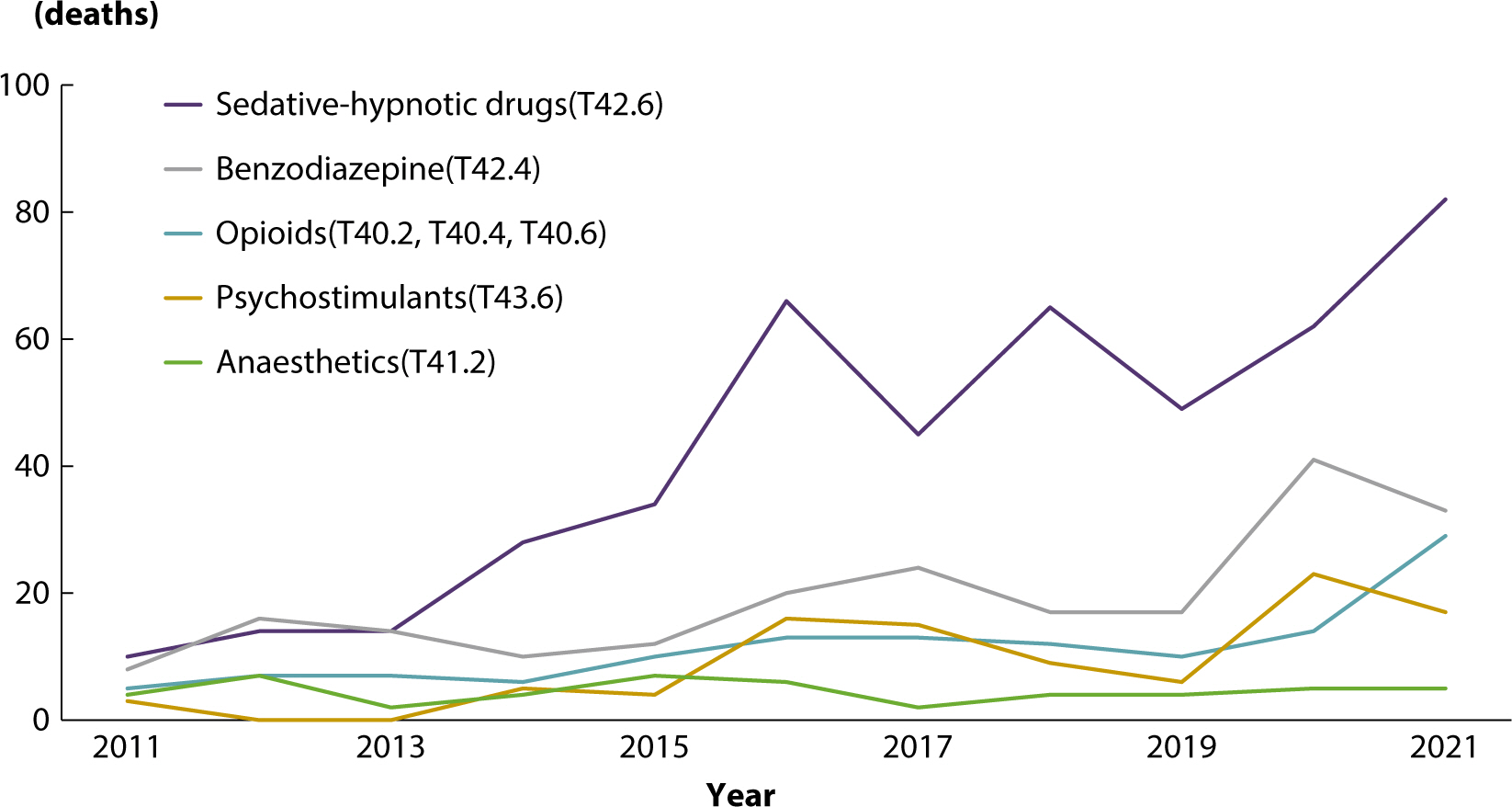
Table 2.The number of deaths due to medical narcotics by age group between
2019 and 2021 (unit: deaths)
|
Age group |
Opioids (T40.2, T40.4, T40.6) |
Anesthetics (T41.2) |
Benzodiazepine (T42.4) |
Sedative-hypnotic drugs (T42.6) |
Others (T41.1, T42.3, T43.6, T48.3,
T50.5) |
|
15−24 |
1 |
2 |
7 |
3 |
8 |
|
25−34 |
12 |
6 |
7 |
16 |
7 |
|
35−44 |
14 |
4 |
8 |
19 |
15 |
|
45−54 |
11 |
2 |
17 |
31 |
16 |
|
55−64 |
8 |
0 |
22 |
42 |
6 |
|
65−74 |
4 |
0 |
13 |
42 |
3 |
|
75−84 |
0 |
0 |
12 |
29 |
- |
|
≥85 |
3 |
0 |
5 |
11 |
- |
Among deaths attributed to medical narcotics, psychostimulants and opioids
represented a significant percentage of accidental fatalities. In instances of
intentional self-harm, sedative-hypnotic drugs and benzodiazepines were commonly
employed. Specifically, sedative-hypnotic drugs constituted 56.7% of
drug-related intentional self-harm cases (Supplement 4).
To analyze the risk of death associated with the use of medical narcotics, the
number of health insurance claims for narcotics was compared to the number of
deaths. For both opioids and psychotropic drugs, the proportion of deaths
relative to the number of claims is higher in younger age groups, indicating
that the risk of death from narcotic drugs is comparatively high among the
young. Specifically, the number of deaths relative to the number of opioid
claims in the 25−44 age group represents a higher proportion compared to
other age groups (Supplement 5).
Discussion
Key results
In 2021, there were 559 drug-induced deaths, marking a 172.7% increase from the
205 deaths recorded in 2011. The rate of drug-induced deaths per 100,000 people
rose to 1.1 in 2021, up 153.6% from 0.4 in 2011. Of the drug-induced deaths in
2021, 75.0% were due to intentional self-harm, and 10.4% were accidental. Deaths
attributed to medical narcotics reached 169 in 2021, a significant increase, up
5.5 times from 31 in 2011. The most commonly involved drugs in these fatalities
were sedative-hypnotic drugs, benzodiazepines, and opioids.
Interpretation
While most deaths occur between the ages of 80 and 84, the majority of
drug-related deaths took place in individuals under the age of 64 (
Fig. 2). This suggests that deaths due to
drugs often result in premature mortality compared to other causes, thereby
disproportionately increasing the disease burden. Furthermore, there has been a
significant rise in the risk of death among younger age groups over the past
decade. Given that 75% of drug-related deaths are due to intentional self-harm
(
Fig. 3), it is evident that
intentional self-harm involving drugs has significantly contributed to the
increased mortality rates in this demographic. This trend highlights the
emergence of drug-induced intentional self-harm as a pressing social issue.
Deaths due to medical narcotics have increased more rapidly than those due to
other drugs (
Fig. 4). Gender differences
were observed in deaths from medical narcotics: men were more likely to die from
drugs with stimulating effects, while women were more likely to die from drugs
with sedative effects. The types of medical narcotics associated with the
highest mortality rates also varied by age, reflecting the fact that the most
commonly prescribed drugs and treatments differ across age groups (Supplement
5). Notably, benzodiazepines were disproportionately involved in deaths among
the young age group of 15 to 24 years old (
Table
2). Because opioids are often used as painkillers for terminal cancer
patients, there are limited medical applications of opioids in younger age
groups. However, there are two potential reasons for the relatively high risk of
opioid-related deaths among young people. The first is the misuse of narcotic
drugs, where death results from intentional misuse without adhering to
prescribed dosages or methods of administration. The second involves medication
being obtained through illegal distribution or purchase, rather than being
prescribed through a legitimate health insurance system. To conduct a thorough
analysis, it is essential to prepare big data linking narcotic drug
prescriptions to death data.
Among medical narcotics, drugs with sedative effects—including
sedative-hypnotic drugs, anesthetics, and benzodiazepines—are frequently
used for intentional self-harm (Dataset 1). Therefore, these drugs require
special management. When comparing the number of health insurance claims to the
number of deaths associated with medical narcotics, the ratio for individuals
aged 25−44 was notably high (
Table
2). This indicates an elevated risk of death in this younger age
group, necessitating targeted management and policies to reduce drug-related
deaths.
No previous articles have reported drug-induced death statistics in Korea. As
drug addiction becomes an increasingly significant social issue in many
countries, including the United States, the need for robust statistics to inform
related policies is becoming more apparent. In the United States, the
age-standardized drug-induced death rate for the total population increased by
29.4% from 22.8 in 2019 to 29.5 in 2020 [
2]. The European Union has developed an estimation model to address the
problem of undercounting drug-related deaths [
4].
Lack of statistical indicators related to drug-induced deaths
The need for policy support to address drug-related deaths is growing, yet
there is a significant shortage of statistical indicators that can determine
the extent and risk factors associated with these fatalities. This scarcity
of statistical indicators for drug-induced deaths stems from three primary
factors.
The first issue is the incompleteness of the criteria used to classify deaths
caused by drugs. Typically, the management of drug distribution and
prescriptions is governed by the Anatomical Therapeutic Chemical
Classification (ATC) codes, which are designated by the Collaborating Center
for Pharmaceutical Statistics Methods (WHOCC), an affiliate of the WHO. Each
ATC code is structured into five levels: drug application site, drug
efficacy, drug characteristics, chemical properties, and individual
ingredients. This detailed classification system facilitates the specific
categorization of drugs, such as opioid-related drugs and benzodiazepines.
However, when classifying causes of death, the ICD-10 from the International
Standard Classification System (WHO-FIC), another affiliate of the WHO, is
utilized. The data on the number of deaths derived from ICD-10 codes is not
without its limitations. Due to inconsistencies in code ranges, deaths
caused by drugs other than narcotics are inadvertently included. For
instance, the T48.3 code, which denotes poisoning by cough medicine,
encompasses drugs other than the medical narcotics dextromethorphan and
zipeprol. Nonetheless, the risk of death and addiction is significantly
higher with medical narcotics than with other general drugs. Additionally,
the T43.6 code, which refers to intoxication by psychostimulants with abuse
potential, primarily includes methylphenidate, a legal drug used to treat
attention deficit–hyperactivity disorder, and methamphetamine, an
illegal substance. The ICD-10 coding system’s limitations in terms of
the details of drug classification suggest that there is potential for
further subdivision in the upcoming revised ICD-11. Thus, the classification
systems for drug prescriptions and causes of death differ significantly,
particularly in that the cause-of-death codes do not adequately classify
drugs in detail.
The second factor is the scarcity of data regarding drug-induced deaths.
While drug prescriptions are well-documented, including details about the
recipient, the dosage, and the specific medications prescribed, information
about drug-related deaths can typically only be obtained through an autopsy
or toxicology testing. Furthermore, elderly individuals often take various
medications for multiple conditions, and it is not uncommon for younger
people to intentionally consume multiple drugs.
Third, there is a lack of linked data spanning prescriptions, illnesses, and
deaths. It is crucial to determine whether drug-related deaths are due to
acute or chronic poisoning. Furthermore, the underlying diseases and health
status of the deceased should be taken into account to accurately assess the
impact of the drug on mortality. Therefore, analyzing data that connects
prescriptions, illnesses, and deaths is essential. By examining linked data,
it would be possible to empirically ascertain the risk of death associated
with a drug by comparing its risk and efficacy against the number of people
prescribed the drug or the dosage prescribed.
Because cause-of-death statistics must adhere to the standards set by the
WHO, analyses involving multiple drugs or drug efficacy, which are necessary
for drug death statistics, are not suitable. Therefore, new, separate
statistics are required to accurately identify the characteristics of deaths
caused by drugs.
How to improve drug-related death statistics
The target population for these statistics is defined as Korean citizens
whose deaths are associated with drugs. Determining whether drugs are
related to a death is only possible through autopsy results; therefore, the
actual population is defined as those cases where drugs were detected in
autopsies conducted by the National Forensic Service. To develop new
statistics using autopsy data, it is essential to establish standards for
classifying drugs. In the statistics for drug-induced deaths among Koreans,
the statistical classification (ATC code) used for drug prescription and
management does not align with the code that classifies the cause of death
(ICD-10). Currently, the ICD-10 does not specify detailed drug types.
Therefore, a linkage table between the ICD-11 and ATC codes must be
developed. To ensure the stability of time series in this linkage table,
ICD-10 codes can be additionally linked to construct statistics using a
consistent classification system from the drug prescription stage through to
the death stage. By developing statistics that classify autopsy data using
both ATC codes and ICD-11 codes, it becomes possible to analyze not only the
efficacy and type of drugs but also the risks associated with polypharmacy.
With detailed classification of drug types, it would be feasible to
construct linked big data that spans drug prescription, disease prevalence,
and death.
Data sources for linked big data necessitate the integration of health
insurance claim details, autopsy data, and cause-of-death statistics. These
linked datasets can serve as empirical evidence for analyzing drug death
risks and drug safety. Specifically, when multiple drugs are consumed, it is
possible to analyze further that the risk of death may increase due to
synergistic effects.
Among many countries, the method Australia uses to compile cause-of-death
statistics is similar to that of Korea, making drug-induced death statistics
from Australia highly relevant to Korea. Generally, drug-related deaths are
prone to underestimation; however, the reliability of these statistics is
enhanced in Australia by incorporating the coroner’s approval
process, and in Korea by including both autopsy results and police
investigations in the statistical compilation [
5,
6]. Australia
has compiled statistics on drugs and opioids and has implemented targeted
policies, which have led to a decrease in mortality rates.
Conclusion
As drug prices fall and online transactions on platforms like the dark web and
cryptocurrency become more prevalent, making them difficult to trace, the risk of
drug-related deaths has increased. This is compounded by a rise in the overseas
inflow of drugs. Therefore, statistical indicators that can be used to establish and
evaluate related policies are essential. It is anticipated that this study and
further in-depth analysis will facilitate the development of future research that
will identify population groups at risk for drug use, provide targeted educational
support, and establish guidelines, ultimately helping to reduce the risk of
premature death due to drugs.
Authors' contributions
-
All work was done by Seokmin Lee.
Conflict of interest
-
No potential conflict of interest relevant to this article was reported.
Funding
-
Not applicable.
Data availability
-
Raw data are available from microdata on cause of death statistics from
Statistics Korea from 2011 to 2021 at https://mdis.kostat.go.kr/index.do
Data files are available from Harvard Dataverse: https://doi.org/10.7910/DVN/D3CXBJ
Dataset 1. Drug-induced deaths, including deaths due to medical narcotics, from
2011 to 2021 by sex, age, type of death, marital status, and educational
attainment provided by Statistics Korea
Acknowledgments
Not applicable.
Supplementary materials
-
Supplementary materials are available from: https://doi.org/10.12771/emj.2024.e27.
Supplement 1. ICD-10 codes for causes of death due to drugs
Supplement 2. The number of deaths and death rate due to drugs by sex and age
Supplement 3. The ranking of deaths due to drug characteristics between 2011 and
2021
Supplement 4. Number of deaths due to medical narcotics by type of death between
2019 and 2021
Supplement 5. Number of deaths compared to the number of medical narcotic
prescriptions by age between 2019 and 2021
Supplement 6. Data used to generate Figs. 1–5
References
- 1. Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: final data for 2020. Natl Vital Stat Rep 2023;72(10):1-92.
- 2. Spencer MR, Miniño AM, Warner M. Drug overdose deaths in the United States,
2001—2021. NCHS Data Brief 2022;(457):1-8. https://dx.doi.org/10.15620/cdc:122556
- 3. Organisation for Economic Co-operation and Development
[OECD]. Addressing problematic opioid use in OECD countries [Internet]. Paris (FR): OECD; c2019 [cited 2023 Oct 4]. Available from https://doi.org/10.1787/a18286f0-en
- 4. Giraudon I, Mathis F, Hedrich D, Vicente J, Noor A. Drug-related deaths and mortality in Europe: update from the EMCDDA
expert network [Internet]. Lisbon (PT): European Monitoring Centre for Drugs and Drug
Addiction; c2021 [cited 2023 Oct 4]. Available from https://doi.org/10.2810/777564
- 5. Australian Bureau of Statistics. Causes of death [Internet]. Canberra (AT): Australian Bureau of Statistics; c2021 [cited 2023 Oct 4]. Available from https://www.abs.gov.au/statistics/health/causes-death
- 6. Australian Bureau of Statistics. Opioid-induced deaths in Australia [Internet]. Canberra (AT): Australian Bureau of Statistics; c2019 [cited 2023 Oct 4] Available from: https://www.abs.gov.au/articles/opioid-induced-deaths-australia