| Erica Kholinne | 5 Articles |
|
[English]
[English]
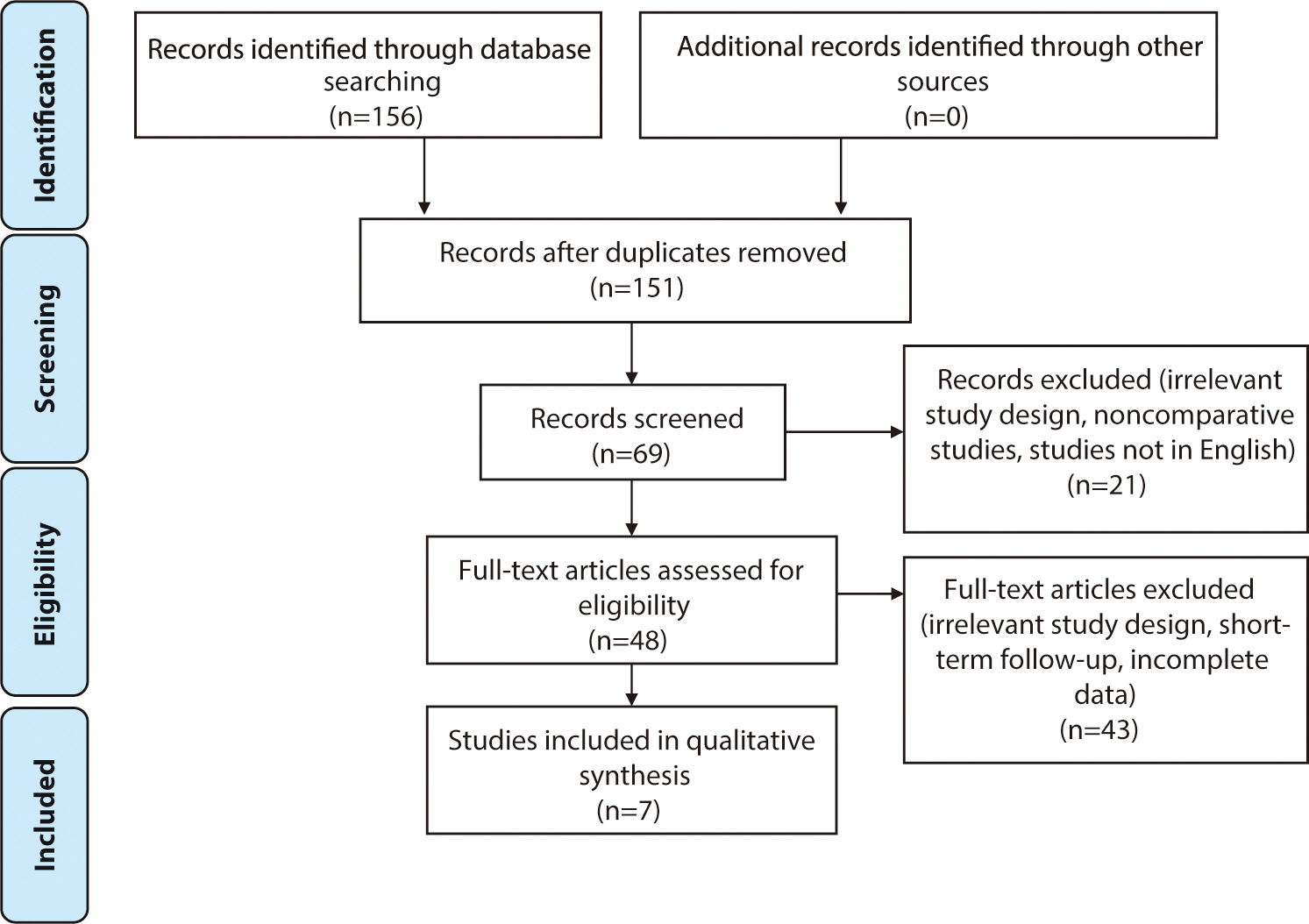
A Bankart lesion is a tear of the labrum, the ring of cartilage that encircles the shoulder joint socket, that can occur when the shoulder is dislocated. This injury frequently affects young athletes and is associated with shoulder instability. This review was performed to provide an overview of anterior shoulder instability, with an emphasis on rehabilitation and the return to sports following arthroscopic Bankart repair. We searched the Google Scholar and PubMed academic databases through February 18th, 2024, utilizing keywords including “arthroscopic Bankart repair” and “return to sports”. Our findings indicate that athletes who undergo arthroscopic Bankart repair exhibit higher rates of returning to sports compared to those who receive other anterior shoulder stabilization procedures. Several factors are considered when determining readiness to return to athletics, including time elapsed since surgery, type of sport, strength, range of motion, pain, and proprioception. Surgeons typically advise athletes to wait approximately 6 months after surgery before resuming sports activities. They also recommend that athletes regain at least 80% of the strength of the uninjured shoulder or achieve strength levels comparable to those prior to the injury. Additionally, patients are expected to attain a full range of motion without pain, which should be symmetrical to the uninjured side, and demonstrate improved proprioception in the shoulder. The sport in which an athlete participates can also influence the timeline for return. Those involved in overhead sports, like baseball or tennis, often experience lower success rates in returning to their sport compared to athletes from other disciplines. Citations Citations to this article as recorded by

[English]
This study aimed to quantify the relationship between proximal humeral rotation and the lateral border of the bicipital groove on fluoroscopic imaging. A composite normal humerus with a marker placed on the lateral border of the bicipital groove was affixed to a custom rotation device at the proximal cut segment. Consecutive fluoroscopic images were captured from −60° to 60° in 5° increments and from −15° to 15° in 1° increments. The index value was calculated by taking the ratio of the distance from the medial boundary of the proximal humerus to the lateral border of the bicipital groove to the distance between the medial and lateral boundaries of the proximal humerus. The correlation between the humeral rotation and the index value was determined. The index value showed a strong positive linear correlation position during internal rotation of the humerus across the entire range (r=0.998, P<0.001), as well as when the humerus was externally rotated, ranging from 15° of internal rotation to 15° of external rotation (r=0.991, P<0.001). The lateral border of the bicipital groove may serve as a useful intraoperative landmark for assessing proximal humeral rotation. This could potentially enhance the outcomes of humeral fracture repair and upper arm arthroplasty.
[English]
ABSTRACT
The review article explores recent advances in the surgical treatment of elbow pain, a common ailment that can significantly impair daily functioning. With a surge in elbow-related conditions such as tennis elbow, osteoarthritis, and nerve compression disorders, the necessity for surgical approaches has become paramount. This article provides an overview of the cutting-edge procedures now available, including minimally invasive arthroscopic surgery. These modern methods have been shown to significantly reduce recovery times and improve overall patient outcomes. The combination of surgical management and targeted rehabilitation ensures a comprehensive and personalized treatment plan for patients with various elbow pathologies. This article aims to shed light on these recent surgical interventions and their potential for advancing the management of elbow pain, emphasizing the ongoing trend toward precision, efficiency, and patient-centered care. Citations Citations to this article as recorded by

[English]
ABSTRACT
Traumatic rupture of the extensor hallucis longus (EHL) is an uncommon finding in an outpatient setting. Surgical repair is typically necessary, particularly in chronic conditions that have persisted for six weeks or more. While several studies have reported EHL repair using autograft tendons, rehabilitation regimes vary, and standardized protocols have not yet been established. This case report presents with an inability to extend her left great toe. She underwent tendon reconstruction with an autograft semitendinosus tendon. At an 8-week follow-up, the patient reported greatly improved outcomes on the American Orthopaedic Foot and Ankle Society, Foot and Ankle Ability Measure, Foot and Ankle Disability Index questionnaire. Full recovery was achieved 12 weeks after surgery. The use of autograft semitendinosus tendon repair for chronic EHL tendon rupture, in conjunction with rehabilitation program, can be expected to yield favorable results.
|
|

