 , Jihyun Ahn
, Jihyun Ahn


Citations

 , YoungMoon Goh
, YoungMoon Goh , Jungwon Kwak
, Jungwon Kwak
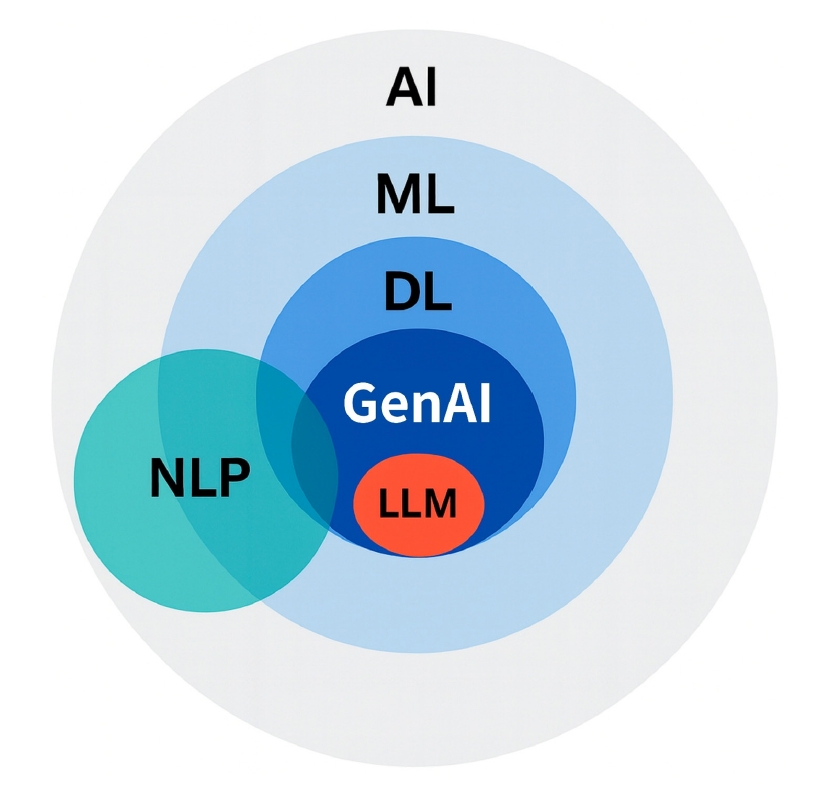
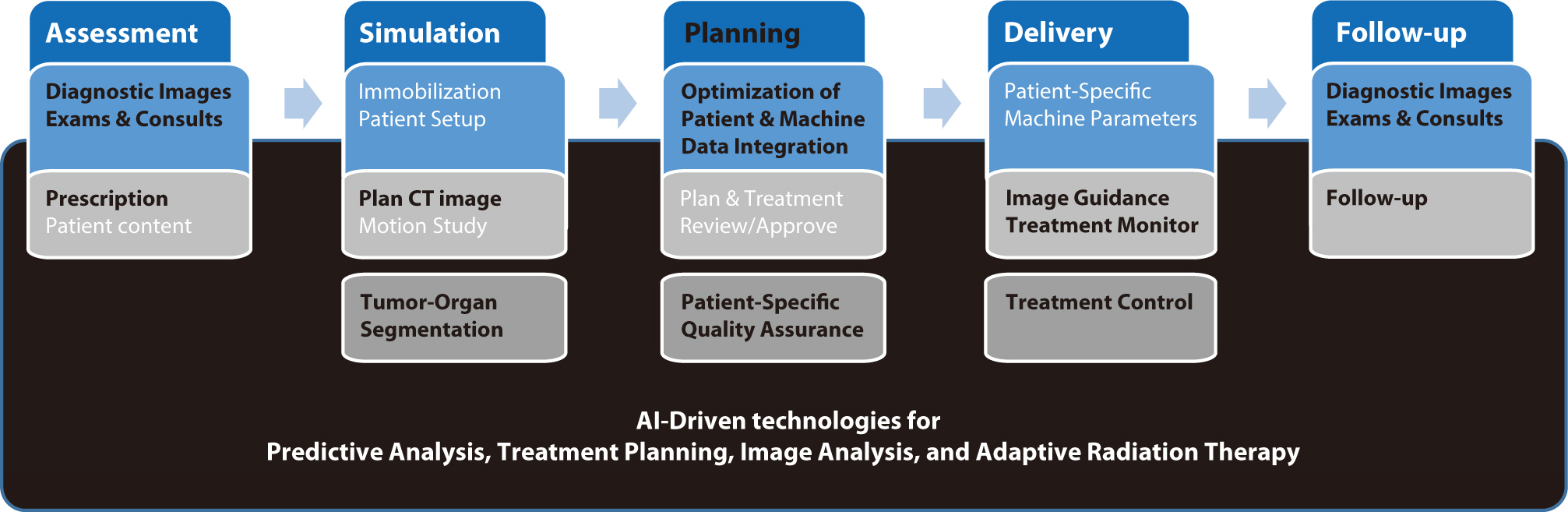
Artificial intelligence (AI) is rapidly transforming various medical fields, including radiation oncology. This review explores the integration of AI into radiation oncology, highlighting both challenges and opportunities. AI can improve the precision, efficiency, and outcomes of radiation therapy by optimizing treatment planning, enhancing image analysis, facilitating adaptive radiation therapy, and enabling predictive analytics. Through the analysis of large datasets to identify optimal treatment parameters, AI can automate complex tasks, reduce planning time, and improve accuracy. In image analysis, AI-driven techniques enhance tumor detection and segmentation by processing data from CT, MRI, and PET scans to enable precise tumor delineation. In adaptive radiation therapy, AI is beneficial because it allows real-time adjustments to treatment plans based on changes in patient anatomy and tumor size, thereby improving treatment accuracy and effectiveness. Predictive analytics using historical patient data can predict treatment outcomes and potential complications, guiding clinical decision-making and enabling more personalized treatment strategies. Challenges to AI adoption in radiation oncology include ensuring data quality and quantity, achieving interoperability and standardization, addressing regulatory and ethical considerations, and overcoming resistance to clinical implementation. Collaboration among researchers, clinicians, data scientists, and industry stakeholders is crucial to overcoming these obstacles. By addressing these challenges, AI can drive advancements in radiation therapy, improving patient care and operational efficiencies. This review presents an overview of the current state of AI integration in radiation oncology and insights into future directions for research and clinical practice.
Citations

 , Ryung-Ah Lee
, Ryung-Ah Lee
The capabilities of artificial intelligence (AI) have recently surged, largely due to advancements in deep learning inspired by the structure and function of the neural networks of the human brain. In the medical field, the impact of AI spans from diagnostics and treatment recommendations to patient engagement and monitoring, considerably improving efficiency and outcomes. The clinical integration of AI has also been examined in specialties, including pathology, radiology, and oncology. General surgery primarily involves manual manipulation and includes preoperative, intraoperative, and postoperative care, all of which are critical for saving lives. Other fields have strived to utilize and adopt AI; nonetheless, general surgery appears to have retrogressed. In this review, we analyzed the published research, to understand how the application of AI in general surgery differs from that in other medical fields. Based on previous research in other fields, the application of AI in the preoperative stage is nearing feasibility. Ongoing research efforts aim to utilize AI to improve and predict operative outcomes, enhance performance, and improve patient care. However, the use of AI in the operating room remains significantly understudied. Moreover, ethical responsibilities are associated with such research, necessitating extensive work to gather evidence. By fostering interdisciplinary collaboration and leveraging lessons from AI success stories in other fields, AI tools could be specifically tailored for general surgery. Surgeons should be prepared for the integration of AI into clinical practice to achieve better outcomes; therefore, the time has come to consider ethical and legal implications.
Citations


