 , Min Young Lee
, Min Young Lee , You Won Choi
, You Won Choi , Hae Young Choi
, Hae Young Choi , Ji Yeon Byun
, Ji Yeon Byun
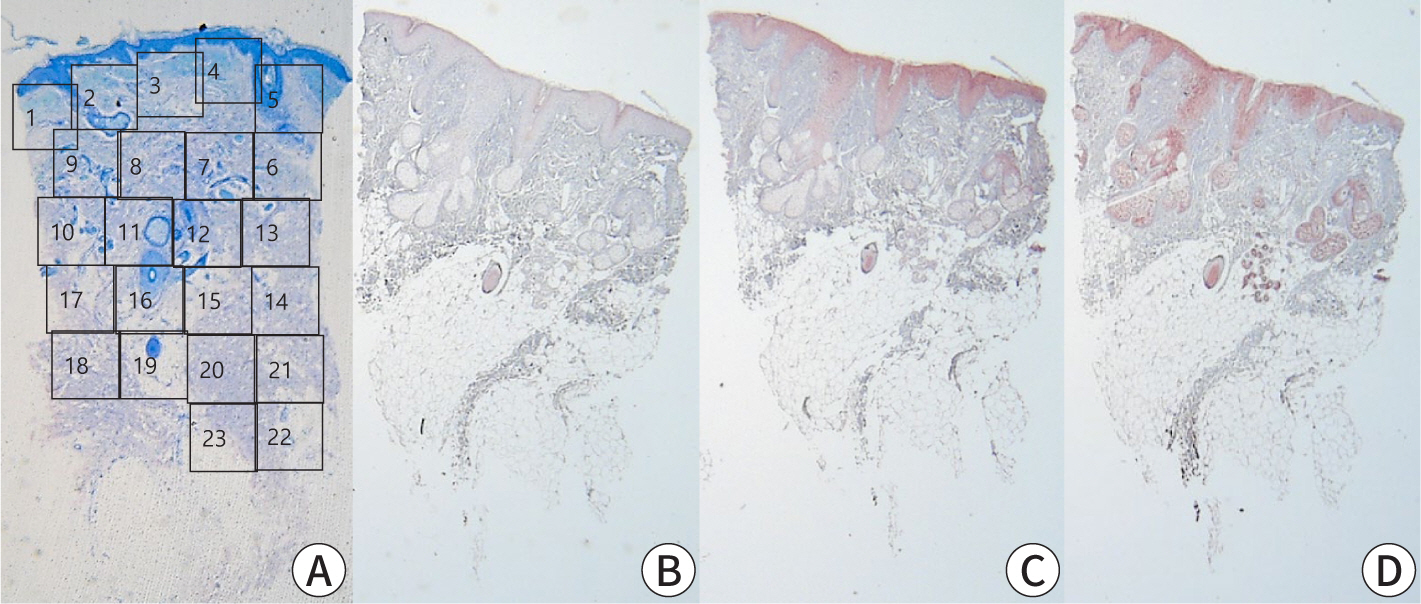
Pancreatic panniculitis is a rare skin complication in which subcutaneous fat necrosis occurs in association with pancreatic disorders, most commonly acute or chronic pancreatitis. Erythematous subcutaneous nodules develop on the legs and spontaneously ulcerate or exude an oily substance. A 32-year-old Korean female patient presented with a 2-week-history of tender nodules with erythematous crusts on her left shin. She had a history of alcoholic liver cirrhosis and, 5 weeks earlier, had been diagnosed with acute pancreatitis. The histopathologic findings from a skin biopsy were consistent with lobular panniculitis, without signs of vasculitis, and diffuse fat necrosis. Basophilic calcium deposits were present in the dermis and subcutaneous fat. These findings were suggestive of pancreatic panniculitis. The skin lesion had a chronic course corresponding to repeated exacerbations of the patient’s pancreatitis. Thus, in the differential diagnosis of subcutaneous nodules, clinicians should consider pancreatic panniculitis as a cutaneous manifestation of pancreatic disease.
 , Ji Seon Chae
, Ji Seon Chae , Minjin Lee
, Minjin Lee , Bo Kyung Kang
, Bo Kyung Kang , Hahck Soo Park
, Hahck Soo Park , Won-Joong Kim
, Won-Joong Kim
An 84-year-old woman visited our pain clinic with complaints of low back pain and severe radiating pain in the right lower extremity during walking. The patient demonstrated subacute compression fracture of L3 with vacuum change in lumbar spine plain radiographs and MRI which suggest Kummell’s disease. Despite our conservative treatments, she had little back pain relief. Therefore, we planned a percutaneous vertebroplasty. Manual compression could help perform percutaneous vertebroplasty more effectively by expanding the vertebral body. In addition, the spontaneous recovery of vacuum cleft width using negative pressure could help perform the technique more effectively. We successfully performed percutaneous vertebroplasty using these combination therapies for our patient.
 , Hae Young Choi
, Hae Young Choi , Ki Bum Myung
, Ki Bum Myung , Eun Ae Park
, Eun Ae Park
Subcutaneous fat necrosis of the newborn is a spontaneously regressing disorder of healthy fullterm of postterm infants, characterized by symmetric, firm, erythematous to violaceous sub-cutaneous nodules and plaques. Histopathologically, subcutaneous fat necrosis with granu-lomatous panniculitis and needle-shaped clefts in the cytoplasm of foamy and multinucleated histiocytic giant cells are diagnostic.
We report an uncomplicated case of subcutaneous fat necrosis in a 21-day-old, normally delivered male infant, which developed on the fourth day of life and spontaneously regressed in 4 months.
 , Ki-Nam Shim
, Ki-Nam Shim , Hyoung Won Cho
, Hyoung Won Cho , Ju Young Choi
, Ju Young Choi , Shin A Lee
, Shin A Lee , Min Jin Lee
, Min Jin Lee , Da Yeon Oh
, Da Yeon Oh , Sun Hee Roh
, Sun Hee Roh , Chung Hyun Tae
, Chung Hyun Tae , Seong-Eun Kim
, Seong-Eun Kim , Hye-Kyung Jung
, Hye-Kyung Jung , Tae Hun Kim
, Tae Hun Kim , Sung-Ae Jung
, Sung-Ae Jung , Sun Young Yi
, Sun Young Yi , Kwon Yoo
, Kwon Yoo , Il Hwan Moon
, Il Hwan Moon
Ingestion of corrosive substances can produce severe injury to the gastrointestinal tract and can even result in death in the acute phase. The extent and degree of damage depends on the type and amount of substances. There are occasional reports of severe contiguous injury to the esophagus and stomach caused by strong alkali ingestion in the acute phase. Usually the deaths occur within a couple of days due to multi-organ failure after ingestion of relatively much amount of agent for a suicidal attempt. But death due to late progression is very rare.
We have reported a case of 60-year-old female patient who was diagnosed as corrosive esophagitis after accidental ingestion of strong alkali. Initial endoscopic findings were compatible with IIa-IIa-0(according to Zargar's classification) in the esophagus, stomach and duodenum, respectively. After several weeks of supportive care, her subjective symptoms were much improved during she had been wating for the operation of colon interposition due to esophageal stricture. Metabolic acidosis and thrombocytopenia developed abruptly probably due to upper gastrointestinal tract necrosis and she died when 60 days had passed after the occurrence of initial esophageal injury.
Citations


Acetaminophen is a mild analgesic and antipyretic agent that is safe and effective when taken in therapeutic doses. Ingestion of overdoses, however, may lead to acute liver failure accompanied by centrilobular degeneration and necrosis. The toxicity of acetaminophen is generally thought to be caused by direct interaction of its reactive metabolites with cellular macromolecules. Cell death, defined as an irreversible loss of vital cellular function and structure, can occur by either necrosis or apoptosis. Until recently, investigation into liver cell death has focused on cell necrosis although it is now appreciated that both apoptosis and necrosis may contribute to liver cell death. The present study examined cultured NCTC-1469 cells for LDH release and DNA laddering and their association with cell death. NCTC-1469 cells were cultured in NCTC-135 medium containing 10% horse serum for 72hr, and changed medium to fresh medium containing acetaminophen(from 0,5mM to 5mM). Cell viability was examined by MTT method and cell necrosis was assessed lactate dehydrogenase leakage. Genomic DNA fragmentation was assessed qualitatively by 1.5% agarose gel electrophoresis. Acetaminophen decreased MTT levels(p<0.05) and increased release of LDH(p<0.05) in dose-dependendent manner. Agarose gel electrophoresis revealed a "ladder" of DNA fragments in all acetaminophen concentration. Cell viability strongly correlated with cell necrosis(r2=0.946). These results show that acetaminophen induced both necrosis and apoptosis in NCTC-1469 cells and cell death mainly attributed to apoptosis.
 , Gyu Bock Choi
, Gyu Bock Choi , Duk Hee Kang
, Duk Hee Kang , Kyun Il Yoon
, Kyun Il Yoon
Acute bilateral renal cortical necrosis is a rare cause of acute reanl failure, occuring in about 2% of patients and it's prognosis is fatal. The pathophysiology of this condition is complex, but ultimately leads to the destruction of the renal cortex with sparing of the renal medulla and a thin tissue rim of under the capsule.
In this report we describe a 23-year-old female patient in whom the diagnosis was made using MR imaging during the acute initial phase of the disease. On T1-weighted images, the signal intensity of the renal cortex was increased, but the signal intensity of the renal cortex was demarcated by a rim of low signal intensity in the region of the corticomedullary junction. MR imaging is useful, noninvasive, and specific modality for an early diagnosis of acute bilateral renal cortical necrosis.

