Deptartment of Oral and Maxillofacial Surgery, Ewha Womans University Mokdong Hospital, Seoul, Korea.
1Division of Oral and Maxillofacial Surgery, Department of Dentistry, Ewha Womans University School of Medicine, Seoul, Korea.
Copyright © 2013. Ewha Womans University School of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
MRA, mandibular repositioning appliance; CPAP, continuous positive airway pressure; RDI, respiratory disturbance index (event per hour); PCS, propective case series; RCT, randomized controlled trial; NG, not given; NA, not applicable. *Values are presented as mean±standard error of the mean, unless so marked, all other values are mean±standard deviation. †P<0.05 compared with baseline. ‡P<0.05 compared with MRA. Adapted from Mohsenin et al. [26] with permission from ADA Publishing Co.
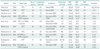

Representative studies presenting the treatment outcomes of MAD and CPAP*
MRA, mandibular repositioning appliance; CPAP, continuous positive airway pressure; RDI, respiratory disturbance index (event per hour); PCS, propective case series; RCT, randomized controlled trial; NG, not given; NA, not applicable. *Values are presented as mean±standard error of the mean, unless so marked, all other values are mean±standard deviation. †P<0.05 compared with baseline. ‡P<0.05 compared with MRA. Adapted from Mohsenin et al. [26] with permission from ADA Publishing Co.
Protocol for treatment with oral appliance.
MRA, mandibular repositioning appliance; CPAP, continuous positive airway pressure; RDI, respiratory disturbance index (event per hour); PCS, propective case series; RCT, randomized controlled trial; NG, not given; NA, not applicable. *Values are presented as mean±standard error of the mean, unless so marked, all other values are mean±standard deviation. †P<0.05 compared with baseline. ‡P<0.05 compared with MRA. Adapted from Mohsenin et al. [