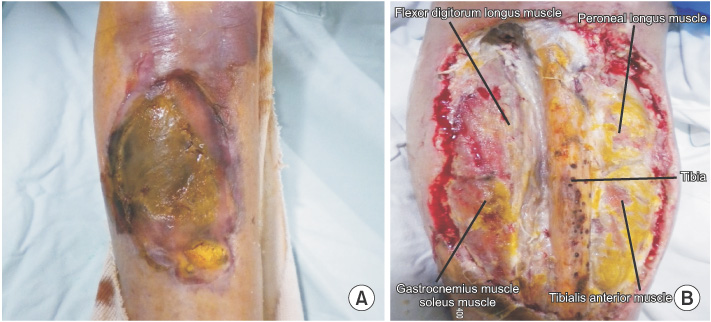
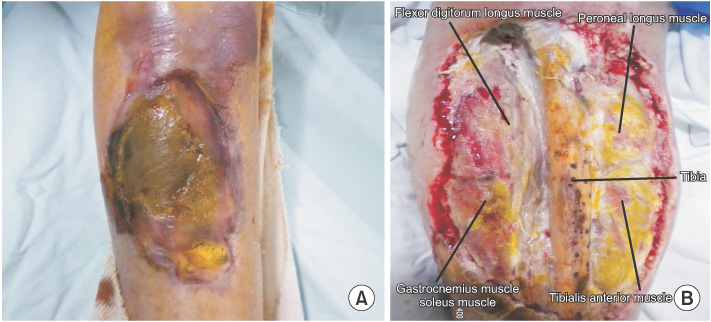
Fig. 1(A) A photograph of the right shin. The tibia is exposed on the front of the right shin accompanying necrotizing tibialis anterior muscle. (B) The picture of the wound during debridement before the surgery. Portions of tibia, tibialis anterior muscle and gastrocnemius muscle are seen. Portions of peroneal longus muscle and soleus muscle are demonstrated, as well.
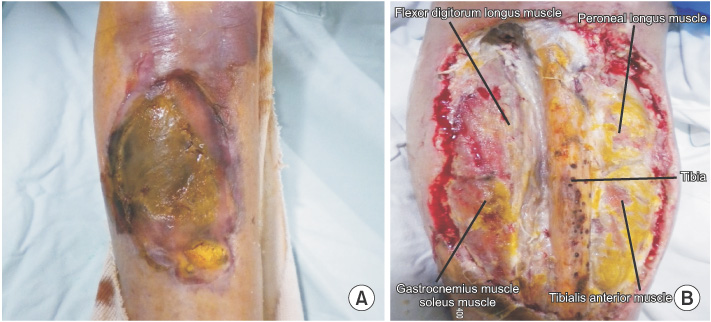
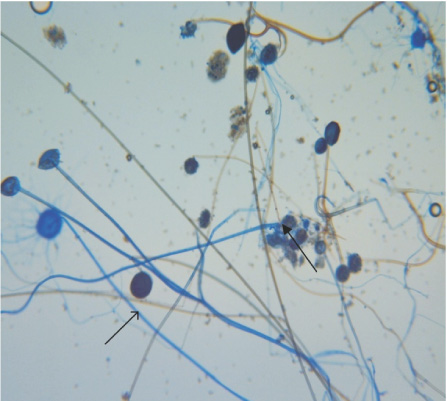
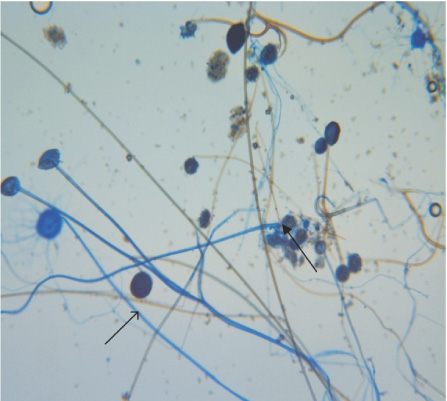
Fig. 2
Rhizopus spp. was found and identified in the experiment cultivating Rhizopus hyphae in pus with debridement which cultivated no septum. It formed a root-shaped hyphae (rhizoid; closed arrow) and an unbranched sporangiospore shaped object (open arrow) at the joining part between the stolon and sporangiospore.
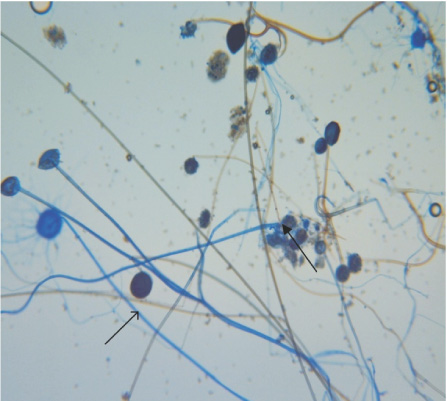
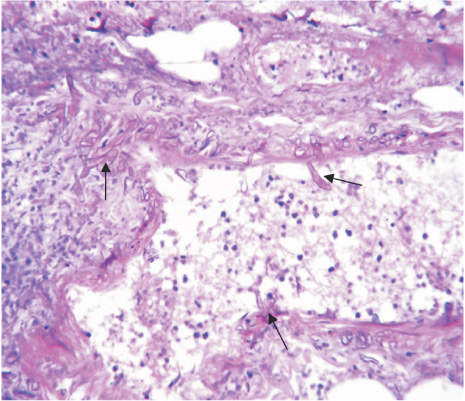
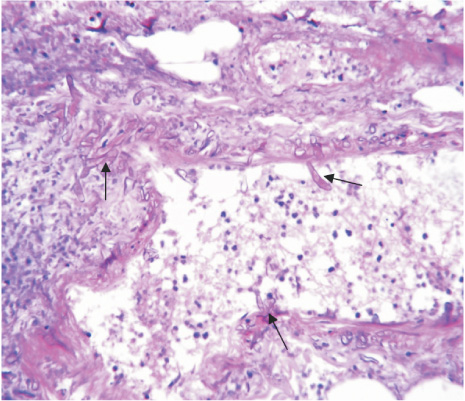
Fig. 3Many zygomycetes (nonseptate, irregularly wide fungal hyphae with frequent right-angle branching; closed arrow) invaded the blood vessel wall (H&E, ×400).