Abstract
Nontuberculous mycobacterial infections, which are often acquired from
environmental sources such as water and soil, exhibit a variety of cutaneous
manifestations that frequently lead to misdiagnoses and delays in treatment. A
77-year-old woman presented with multiple skin lesions in a sporotricoid
distribution on her right leg, which persisted despite standard antibiotic
treatments. Based on the skin biopsy, revealing granulomatous inflammation with
acid-fast bacilli, and PCR testing, a nontuberculous mycobacterial infection was
diagnosed. Antimycobacterial drug combinations, including clarithromycin,
isoniazid, and rifampicin for 4 months, complete the skin lesion's
clearance. This case underscores the need for heightened suspicion and the use
of appropriate diagnostic techniques, including tissue biopsies and molecular
methods such as PCR.
-
Keywords: Anti-bacterial agents; Biopsy; Nontuberculous mycobacteria; Polymerase chain reaction; Republic of Korea
Introduction
Nontuberculous mycobacterial infections are caused by mycobacteria other than
Mycobacterium tuberculosis and
Mycobacterium
leprae. Nontuberculous mycobacteria are commonly found in the
environment, particularly in water and soil, and are more frequently associated with
skin diseases than
M. tuberculosis [
1]. The infections they cause present a broad spectrum of skin symptoms.
Due to this diversity, these infections are often misdiagnosed, leading to delays in
treatment [
2].
Case presentation
Ethics statement
Informed consent for publication was obtained from the patient.
Patient information
A 77-year-old woman presented with multiple skin lesions on her right leg that
had developed approximately 3 to 4 months previously. Aside from hypertension,
she had no significant medical history and no known exposure to water or soil
that might explain her condition.
Clinical findings
A physical examination revealed several erythematous to maroon-colored crusted
deep nodules arranged in a linear pattern on her right leg (
Fig. 1).
Fig. 1.Multiple erythematous to maroon-colored crusted deep nodules were
arranged linearly on the right leg. Informed consent was obtained for
the publication of this case report and accompanying images.

Timeline
She was initially treated for cellulitis, but her condition did not improve.
Therefore, she was referred for further investigation.
Diagnostic assessment
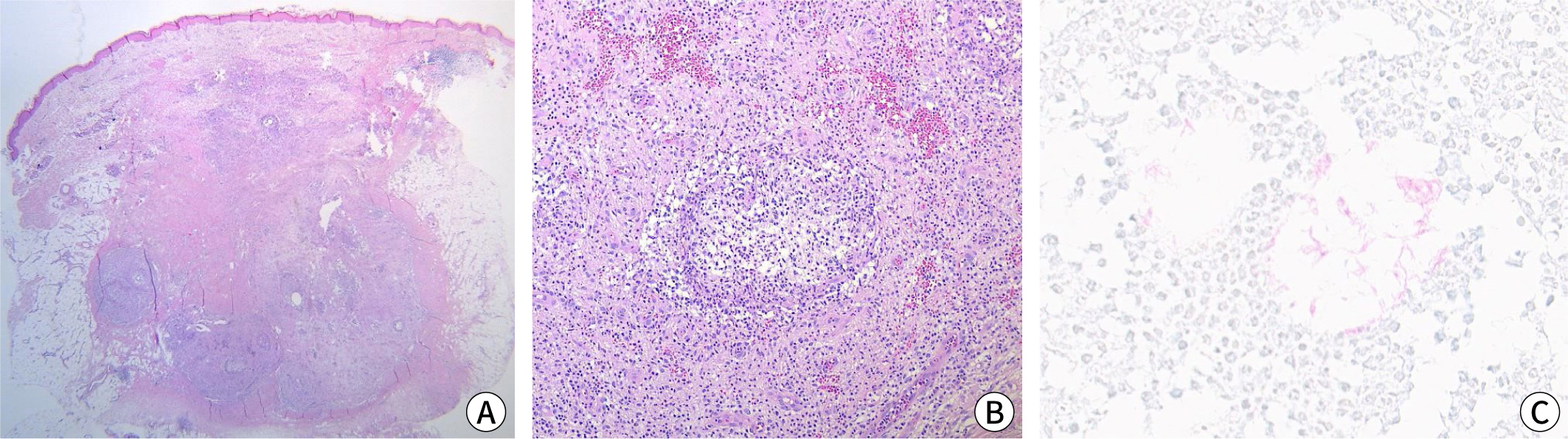
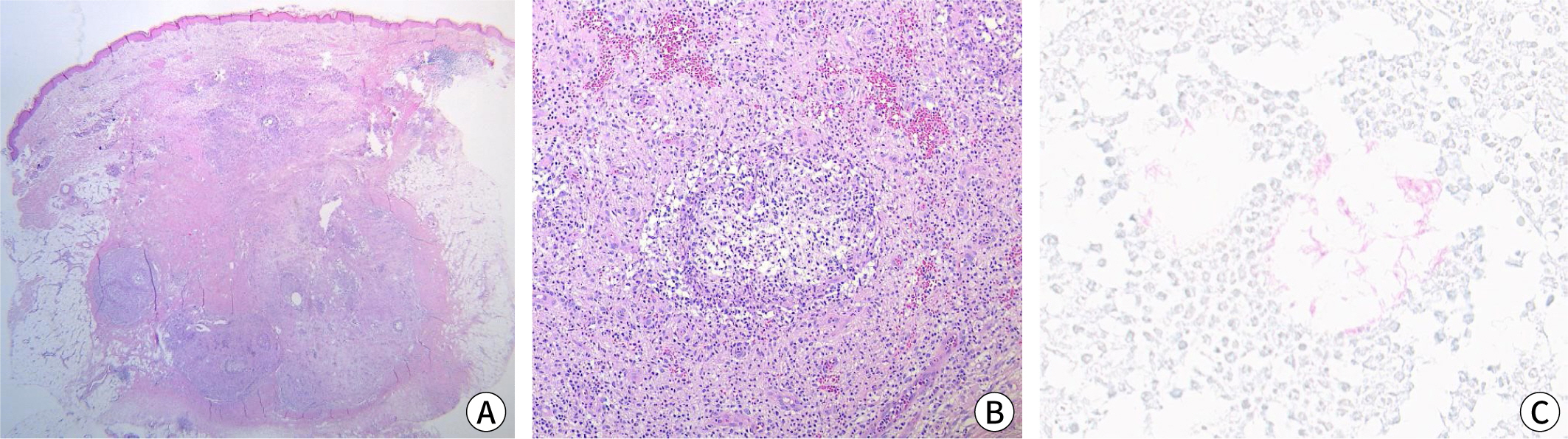
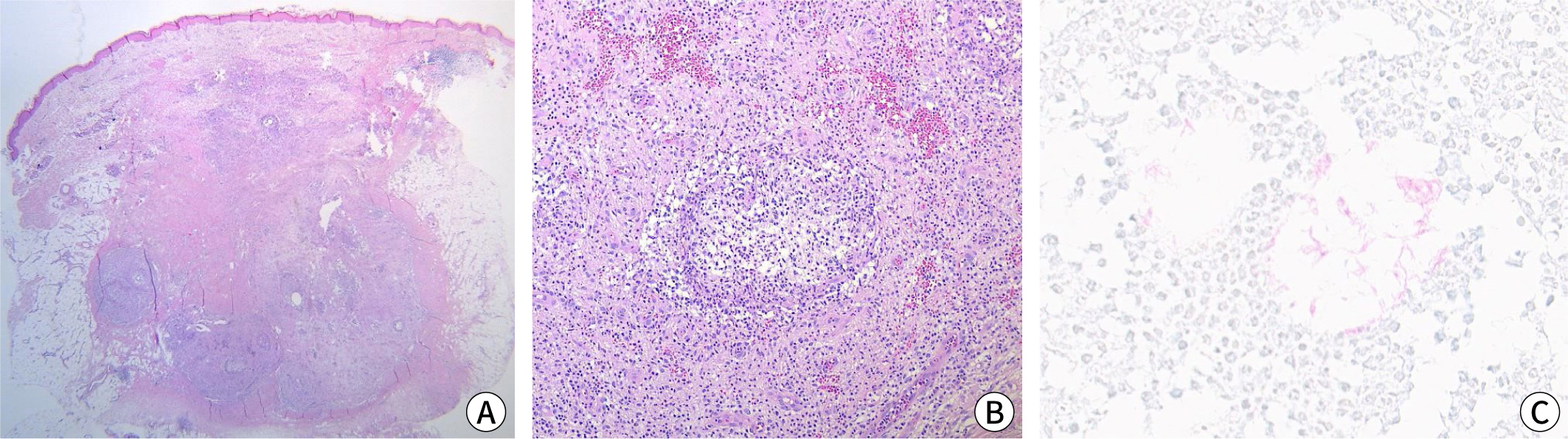
A skin biopsy demonstrated granulomatous inflammation extending deep into the
subcutaneous tissue (
Fig. 2A,
B). Acid-fast bacilli (AFB) were identified
with Ziehl-Neelsen staining (
Fig. 2C). PCR
analysis for mycobacteria was also performed on the tissue specimen, and the
results were positive. We used AdvanSure TB/NTM real-time PCR (LG Chem, Seoul,
Korea); however, this system cannot define the exact type of tuberculosis.
Attempts to culture the nontuberculous mycobacteria, both in a mycobacteria
growth indicator tube and on Lowenstein-Jensen medium, were unsuccessful.
Fig. 2.Histological findings. (A,B) Granulomatous inflammation was observed
in the dermis and subcutaneous tissue (hematoxylin and eosin: A,
×100; B, ×200). (C) The Ziehl-Neelsen stain revealed
acid-fast bacilli (×400). Informed consent was obtained for the
publication of this case report and the accompanying images.
Therapeutic intervention
Treatment began with minocycline (50 mg twice daily), leading to gradual
improvement over 3 months, but was halted due to gray hyperpigmentation at the
treated sites. A switch to clarithromycin (500 mg daily) led to moderate
improvement, but new lesions appeared after 4 months. Therefore, the regimen was
modified to include isoniazid (200 mg per day) and rifampicin (450 mg per day),
leading to noticeable clinical improvement within a month.
Follow-up and outcomes
After 4 months on this regimen, the lesions completely cleared, and no relapse
was noted during a 6-month follow-up.
Discussion
The prevalence of skin infections caused by nontuberculous mycobacteria appears to be
increasing. These infections manifest with a range of cutaneous symptoms, such as
abscesses, cellulitis, sporotrichoid nodules, ulcers, and panniculitis. The diverse
nature of these symptoms makes diagnosis challenging, necessitating a high degree of
suspicion in relevant clinical contexts to ensure timely identification.
Nontuberculous mycobacterial infections should be suspected in patients whose skin
infections are resistant to standard treatments [
3].
Infections that present in a 'sporotrichoid' form are characterized by
multiple lesions along the superficial lymphatic vessels, resembling the
lymphangitis observed in sporotrichosis [
4].
Various mycobacteria, including
Mycobacterium marinum, Mycobacterium
kansasii, Mycobacterium avium complex, and
Mycobacterium
chelonae, are known to exhibit this sporotrichoid pattern [
5].
The diagnosis of mycobacterial infection necessitates tissue biopsies to evaluate the
presence of AFB and to culture tissue specimens. Molecular techniques, such as PCR,
are increasingly utilized to accurately identify mycobacterial pathogens in tissue
samples [
5]. In this instance, AFB were
detected histologically, and nontuberculous mycobacteria were confirmed through PCR,
although the specific organism could not be cultured.
Treatment guidelines recommend susceptibility testing of mycobacterial isolates to
optimize the choice of specific antimycobacterial drug combinations [
5]. Due to the inability to isolate the
causative mycobacterium, empirical treatments were administered, assuming an
M. marinum infection, which typically demonstrates a
sporotricoid pattern. There is no standardized treatment regimen for nontuberculous
mycobacterial infections, owing to the rarity of cases and the absence of controlled
trials. Common regimens for
M. marinum include tetracyclines,
specifically minocycline and doxycycline, trimethoprim-sulfamethoxazole, rifampicin,
and clarithromycin. For resistant cases, a combination of rifampicin and ethambutol
may be employed. The duration of therapy varies based on clinical response and can
last up to 1 year [
6]. It is advised to
continue medication for at least 4–8 weeks after lesions have disappeared
[
7].
In conclusion, we report a case of nontuberculous mycobacterial infection presenting
with a sporotrichoid distribution. Obtaining histopathology and conducting
appropriate culture or molecular tests are essential for making the diagnosis.
Authors' contributions
-
Project administration: Byun JY
Conceptualization: Byun JY, Choi YW, Roh JY, Choi HY
Methodology & data curation: Choi YW, Roh JY, Choi HY
Funding acquisition: not applicable
Writing – original draft: Byun JY
Writing – review & editing: Lee JJ, Choi YJ, Byun JY, Choi YW, Roh
JY, Choi HY
Conflict of interest
-
Ji Yeon Byun has been an associate editor of the Ewha Medical
Journal; however, she was not involved in peer review process or
decision making. No other potential conflict of interest relevant to this
article was reported.
Funding
-
Not applicable.
Data availability
-
Not applicable.
Acknowledgments
Not applicable.
Supplementary materials
-
Not applicable.
References
- 1. Sethi A. Tuberculosis and infections with atypical
mycobacteria. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, editors. editors. Fitzpatrick’s dermatology in general medicine. 9th.ed. New York: McGraw-Hill; 2019 p. 28702871.
- 2. Jogi R, Tyring SK. Therapy of nontuberculous mycobacterial
infections. Dermatol Ther 2004;17(6):491-498.
- 3. Gonzalez-Santiago TM, Drage LA. Nontuberculous mycobacteria: skin and soft tissue
infections. Dermatol Clin 2015;33(3):563-577.
- 4. Weedon D. Weedon’s skin pathology. 3rd ed. London: Churchill Livingstone; 2010 p. 560.
- 5. Franco-Paredes C, Marcos LA, Henao-Martínez AF, Rodríguez-Morales AJ, Villamil-Gómez WE, Gotuzzo E, et al. Cutaneous mycobacterial infections. Clin Microbiol Rev 2018;32(1):e00069-18.
- 6. Palenque E. Skin disease and nontuberculous atypical
mycobacteria. Int J Dermatol 2000;39(9):659-666.
- 7. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and
prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 2007;175(4):367-416.
Figure & Data
Citations
Citations to this article as recorded by

- Clarithromycin
Reactions Weekly.2024; 2014(1): 180. CrossRef