Abstract
-
Objectives: Accurately targeting distal nail holes and placing
distal interlocking screws pose challenges during intramedullary nailing. This
study proposes a straightforward technique for distal locking screw insertion
using a Steinmann pin, eliminating the need to reposition the pin or drill
bit.
Methods: We utilized 18 Sawbones femur models and intramedullary
femur nails. A first-year resident created two distal locking holes on each
model, employing both the conventional freehand technique and a novel method
involving a Steinmann pin and hammer under image intensification. These
techniques were evaluated based on three parameters: (1) the time required to
create distal locking holes, measured from the moment the pin was positioned at
the center of the hole until the far cortex was drilled through the interlocking
hole; (2) the radiation dose (in mrem/h), as estimated with a personal gamma
radiation dosimeter; and (3) the number of failures, defined as the creation of
more than one hole in the near and far cortex.
Results: The new technique was associated with a lower radiation
dose (P=0.0268) and fewer failures (P=0.0367) than the conventional approach.
Additionally, the time required to establish distal holes was shorter using the
new technique compared to the conventional method (P=0.0217).
Conclusion: The creation of distal interlocking holes with a
Steinmann pin and hammer is accurate, efficient, and cost-effective.
-
Keywords: Bone screws; Cost-benefit analysis; Femur; Fracture; Radiation dosage
Introduction
Background/rationale
Intramedullary (IM) nailing is widely used in orthopedic practice and has
recently become the gold standard for treating femoral and tibial diaphyseal
fractures. This method is also occasionally employed for humeral shaft fractures
due to its load-sharing characteristics [
1,
2]. To achieve rotational
stability, surgeons may insert proximal and distal interlocking screws. While
proximal screws are relatively straightforward to place using an aiming device,
the placement of distal screws presents a challenge. This difficulty arises from
the deformation of the nail within the medullary canal, which leads to
misalignment of the distal locking holes. Consequently, distal interlocking
screws must be inserted using a freehand technique.
Targeting the distal nail holes and accurately placing the distal interlocking
screws with a freehand approach can be challenging, even for an experienced
surgeon. This freehand method of distal screw insertion also involves a
radiolucent drive, which may not be available. An alternative is to continuously
monitor the projection of the drill bit’s tip. However, this approach is
difficult and necessitates multiple radiological exposures. Ikpeme et al.
reported that the distal interlocking procedure is time-consuming and increases
the duration of surgery [
3]. If the hole
for the interlocking screw is drilled incorrectly, the pre-existing path can
interfere with the creation of a new hole, as the drill bit may deviate and
slide into the previously drilled hole.
The use of multiple drilling attempts can result in iatrogenic fractures and
increased radiation exposure for both patient and surgeon [
4,
5]. In response,
studies have introduced various modifications to the common freehand technique
[
6–
9]. These approaches primarily involve the use of a smooth
pin that is subsequently removed and replaced with a drill bit or the placement
of a cannulated reamer over the pin. However, procedures that require
reinserting the drill after pin removal are time-consuming and prone to failure
[
10].
In this study, we introduce a straightforward method for the insertion of distal
interlocking screws using a Steinmann pin. This technique eliminates the need
for repositioning the pin or drill bit, offering an accurate and time-efficient
alternative to the conventional method.
Methods
Ethics statement
No institutional review board approval or informed consent was necessary for this
study, as the materials used were commercially purchased Sawbones.
Study design
In this comparative study, we evaluated the accuracy and time efficiency of the
new technique. The findings were reported in accordance with the Strengthening
the Reporting of Observational Studies in Epidemiology (STROBE) statement, which
is accessible at
https://www.strobe-statement.org/.
A first-year resident with no prior experience in inserting distal interlocking
screws experimented on 18 femur Sawbones models (Sawbones, Vashon, WA, USA) with
femoral IM nails (unreamed femoral nail; Synthes, Oberdorf, Switzerland).
Following the insertion of the IM nail and proximal locking screws, the resident
created two distal locking holes using both the conventional freehand technique
and the new method, under image intensifier guidance. The study of this surgical
technique was conducted at Gyeongsang National University Changwon Hospital.
Surgical technique
A Steinmann pin matching the size of the drill bit was utilized; specifically,
1/8-inch (3.2 mm) and 5/32-inch (4.0 mm) Steinmann pins were employed for the
tibia and femur, respectively. In the proposed technique, the Sawbones model is
placed in a supine position on the operating table, with the limb adequately
stabilized. Following thorough sterilization of the surgical site, the C-arm is
positioned to be perpendicular to the limb. This orientation ensures that the
screw holes appear as perfect circles on the fluoroscopic image, a critical
factor for accurate visualization and the success of subsequent procedural
steps.
The entry point for the Steinmann pin is determined with a high level of accuracy
that reflects the precision of the freehand technique. The drill is then
equipped with a Steinmann pin, positioning the tip in direct contact with the
near cortex. To obtain a clear fluoroscopic image without the interference of a
drill shadow, the Steinmann pin is held at an oblique angle to the shaft.
Importantly, the tip of the pin must be precisely centered within the locking
hole. Adjustments can be made in the proximal, distal, anterior, or posterior
directions until optimal centering is achieved. Once the pin is centered, the
drill is aligned parallel to the C-arm X-ray beam, and drilling into the near
cortex begins.
During the drilling process, the drill is periodically tilted to ensure that the
Steinmann pin remains centered in the hole. After confirming the correct
positioning, drilling continues toward the far cortex. If the Steinmann pin
contacts the nail or deviates from its path relative to the hole, the handpiece
is detached from the pin, which remains inserted in the near cortex. The
Steinmann pin is then adjusted by bending or tilting, as directed by
fluoroscopic guidance, to realign it with the hole (
Fig. 1).
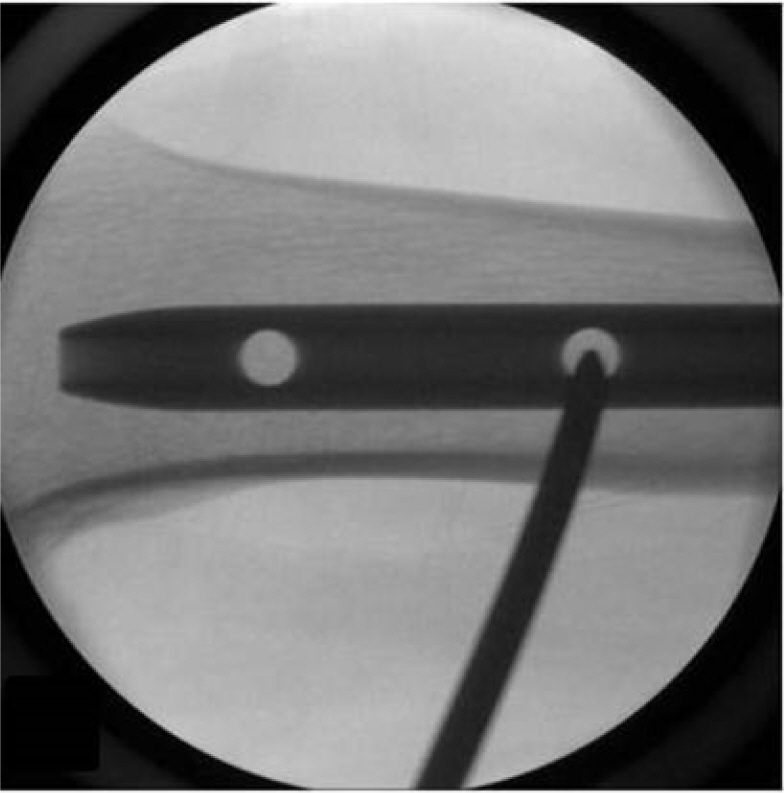
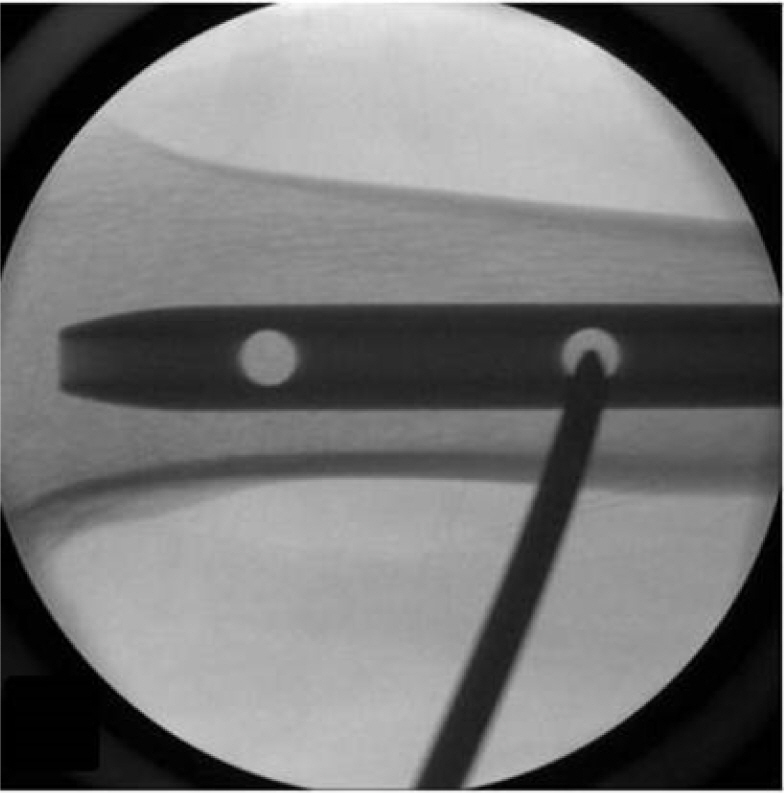
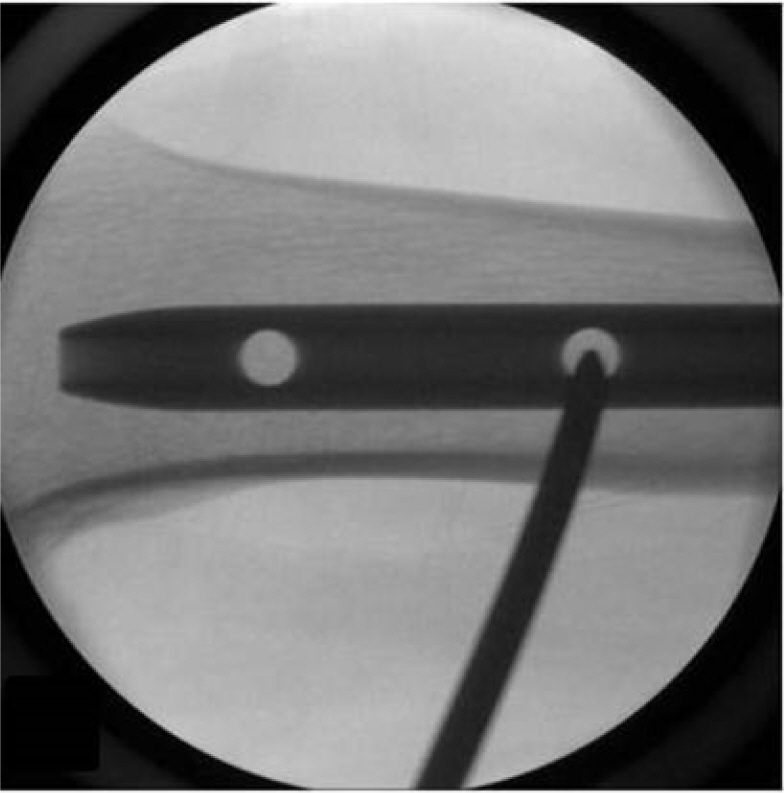
Fig. 1.The drilling machine was detached from the Steinmann pin after
insertion into the near cortex. Subsequently, the pin was bent to align
with the path to the hole, under image intensifier guidance.
Once the orientation is verified, the Steinmann pin is tapped with a hammer to
advance it through the interlocking hole until it reaches the far cortex. Once
in place, the pin is clamped into the drilling machine, and drilling through the
far cortex is completed. An interlocking screw is then inserted through the
newly created hole to ensure secure fixation (
Figs. 2,
3).
Fig. 2.Once the direction was confirmed, the Steinmann pin was tapped into
place with a hammer.

Fig. 3.A Steinmann pin is shown reaching the far cortex after passing
through the interlocking hole.

Finally, the correct placement of the interlocking screw is verified using
fluoroscopy. The surgical site is then closed in accordance with the standard
protocol, and an appropriate dressing is applied. This meticulous technique
increases the precision of distal locking hole placement during IM nailing,
minimizing potential complications and improving surgical outcomes.
Materials
Each of the 18 Sawbones models was utilized for both new and conventional
techniques.
Variables (study outcomes)
The outcome variables included the duration required to perform the surgical
technique, the radiation dose to which the Sawbones were exposed, and the number
of attempts required to successfully execute the technique.
Data sources and measurement
The measurement methods were as follows. (1) The time taken to create the distal
locking holes was recorded. This interval began at the Steinmann’s pin
was positioned at the center of the hole and continued until the far cortex was
drilled through the interlocking hole. (2) Radiation dose (mrem/h) was measured.
A personal gamma radiation dosimeter (EcotestCARD; ECOTEST, Lviv, Ukraine) was
attached to the lead apron worn by the operator to assess the radiation dose
received throughout the entire procedure. (3) The frequency of attempts was
noted, with failure defined as the establishment of more than one hole in the
near and far cortex. The research data are available in Dataset 1.
Bias
This study involved no selection bias, as the same purchased models were used for
both groups.
Study size
Sample size estimation was not performed.
Statistical methods
We compared the results associated with the conventional and new techniques.
Given the absence of normal distribution, all variables were analyzed using
non-parametric statistical methods. The P-value was determined through the
Wilcoxon rank-sum test. For statistical analyses, we utilized DBSTAT 5.0
(DBSTAT, Seoul, Korea), which can be accessed at
http://dbstat.com/.
Results
Participants
The 36 trials involved commercially purchased materials, and no demographic data
were collected.
Main results
Surgical duration
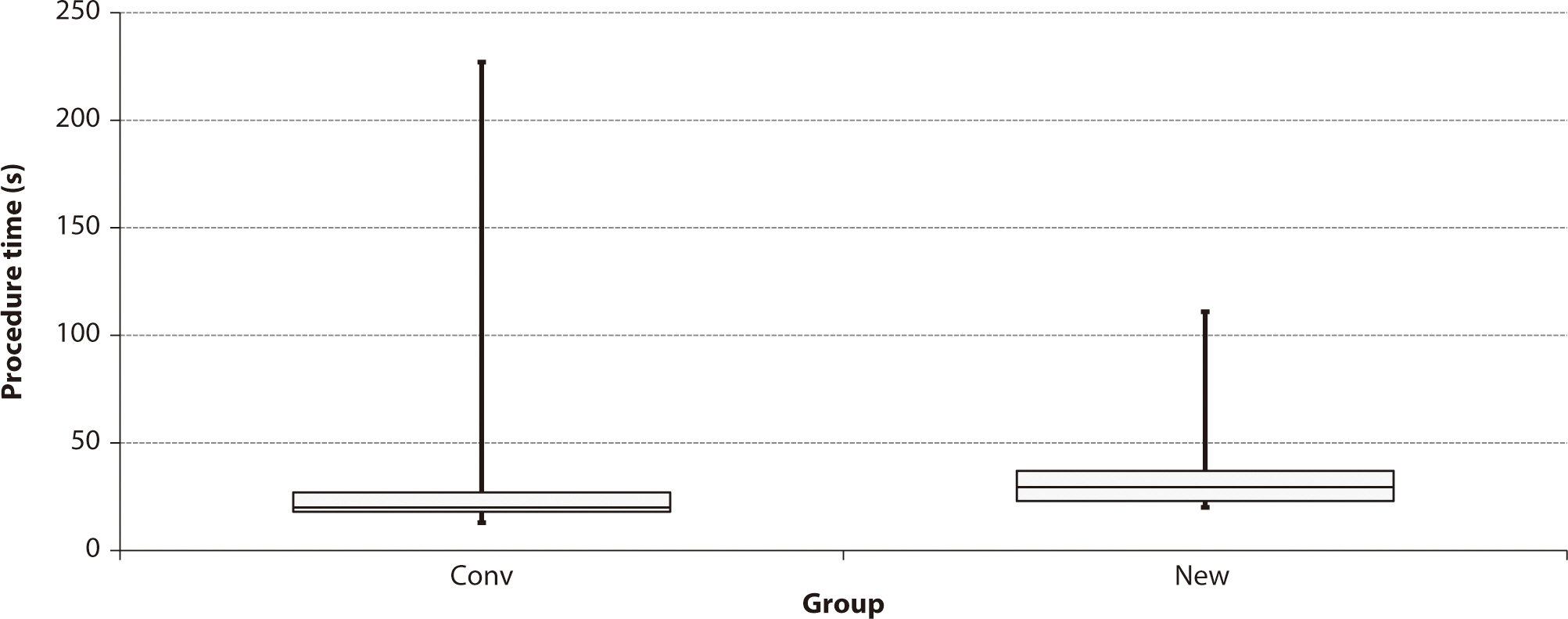
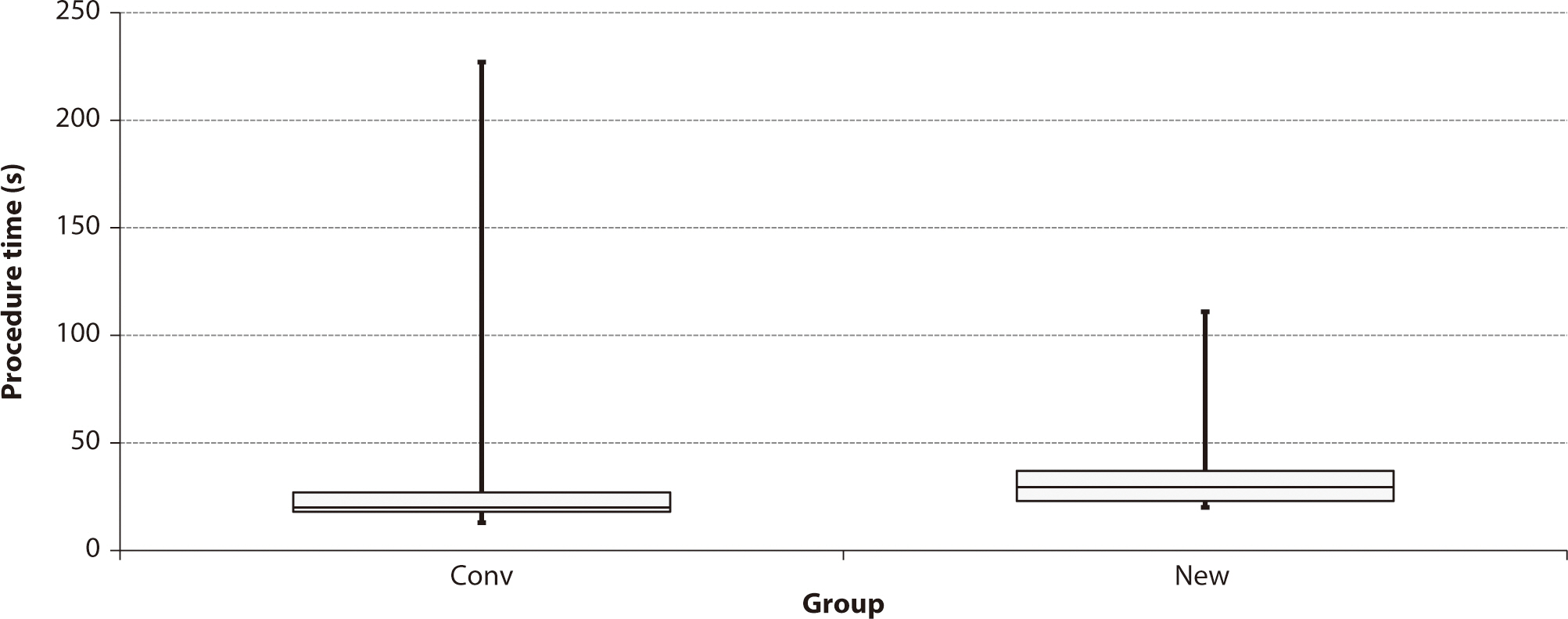
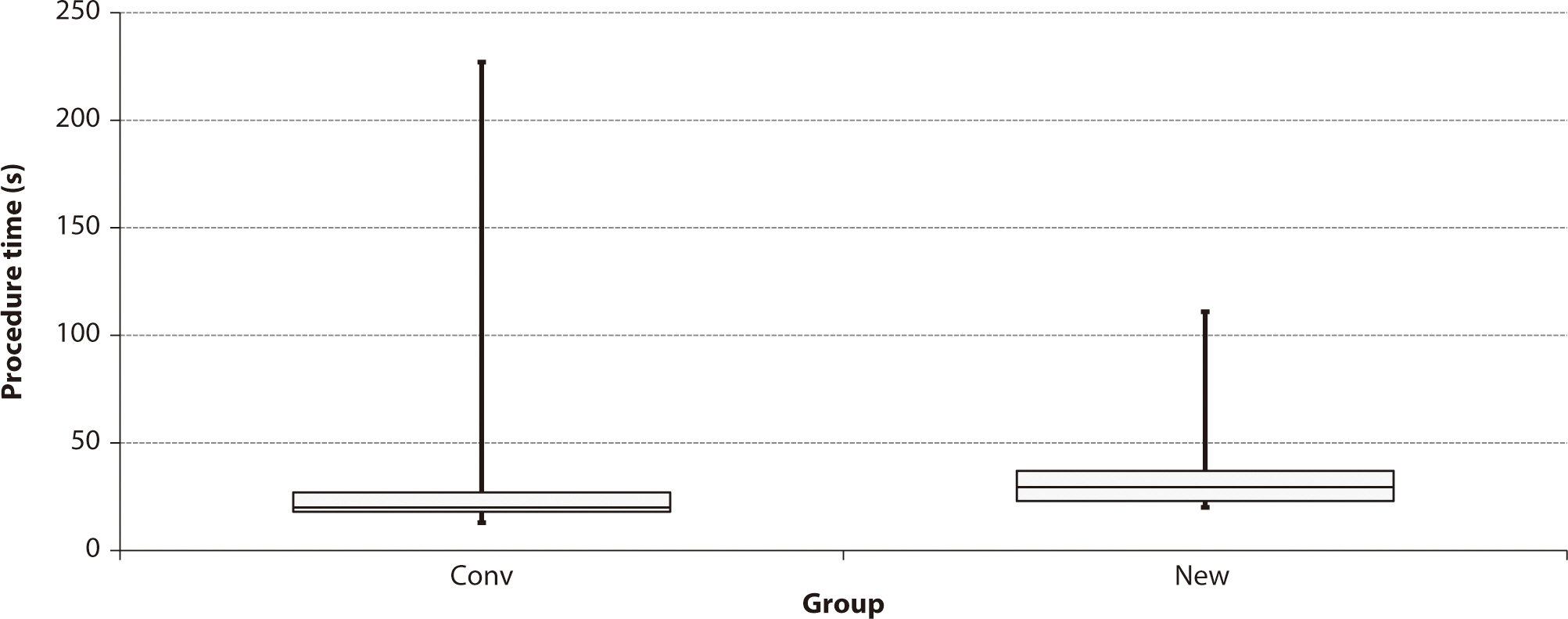
The median times required for the conventional and new techniques were 29.5
and 20.0 seconds, respectively. The difference between groups was
significant (Wilcoxon W=260.5, corrected Z=−2.963, P=0.0217,
Fig. 4).
Fig. 4.Comparison of procedure time between the conventional technique
(Conv) and the new method (New) for intramedullary nailing. Values
are presented in seconds.
Radiation exposure
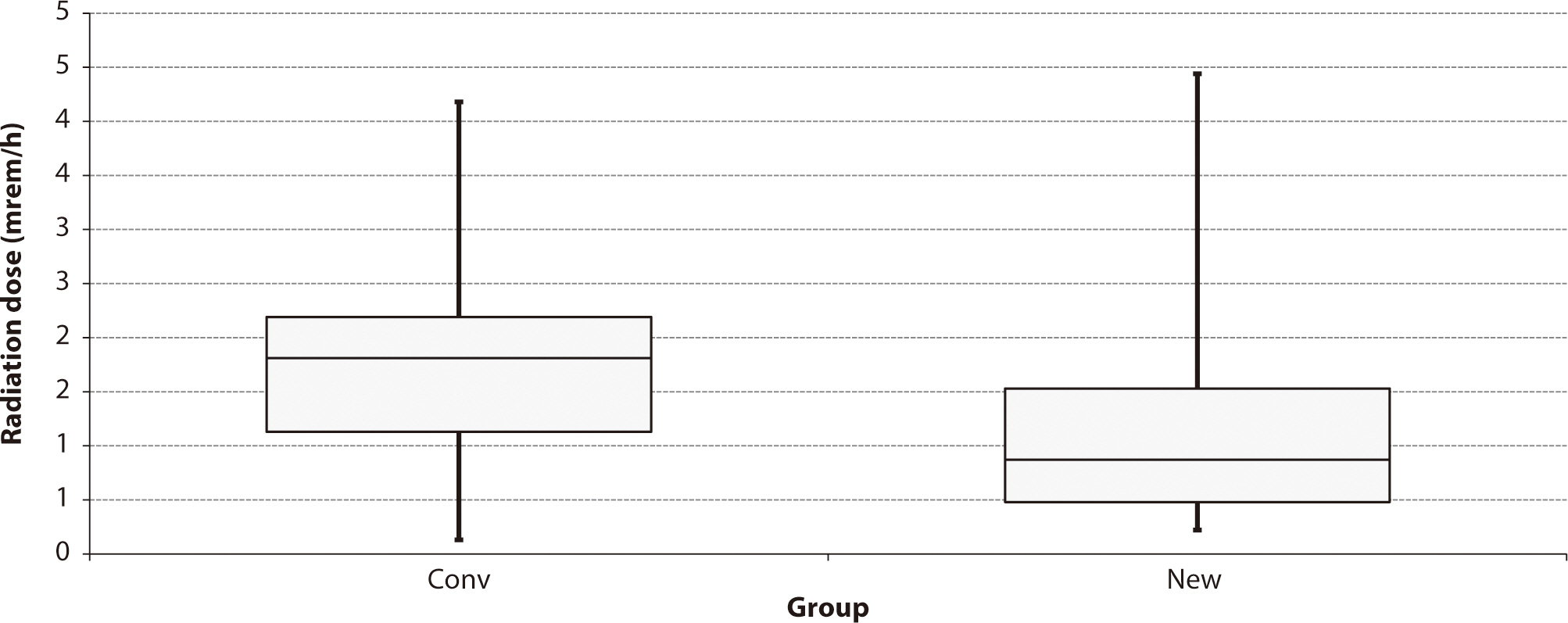
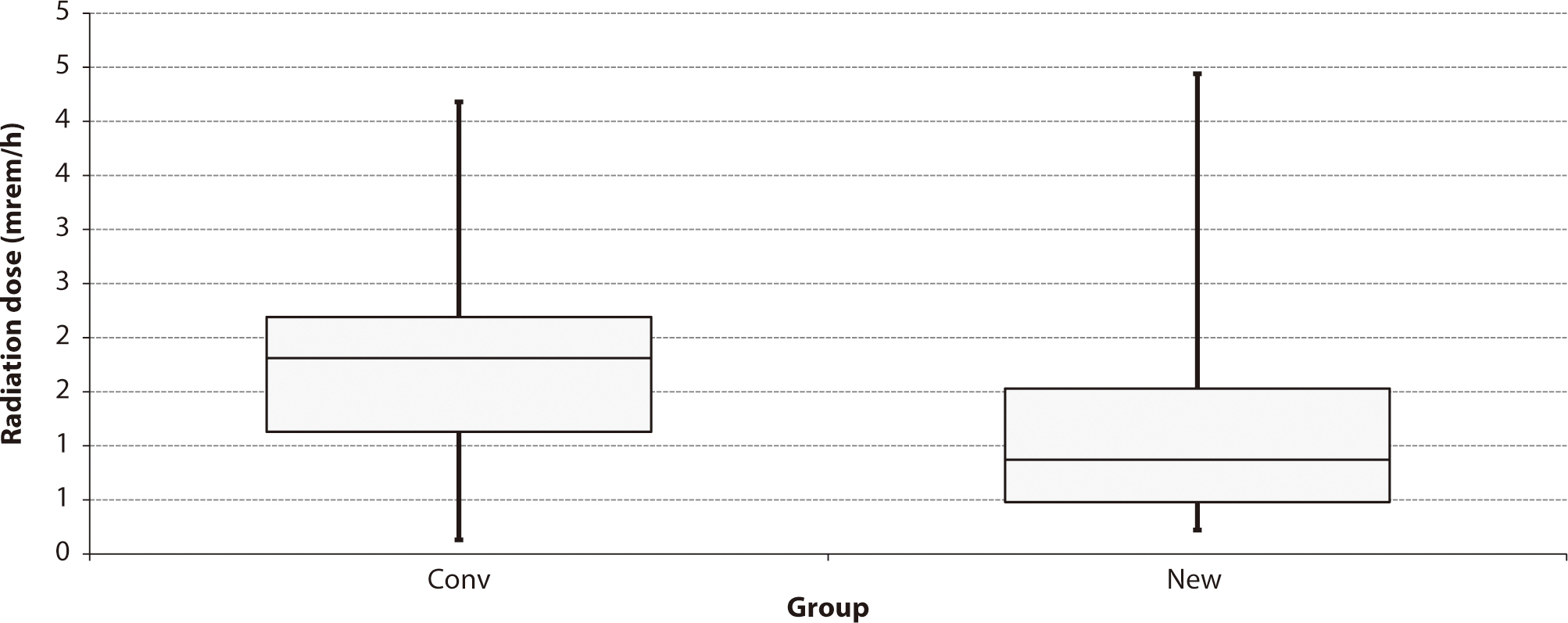
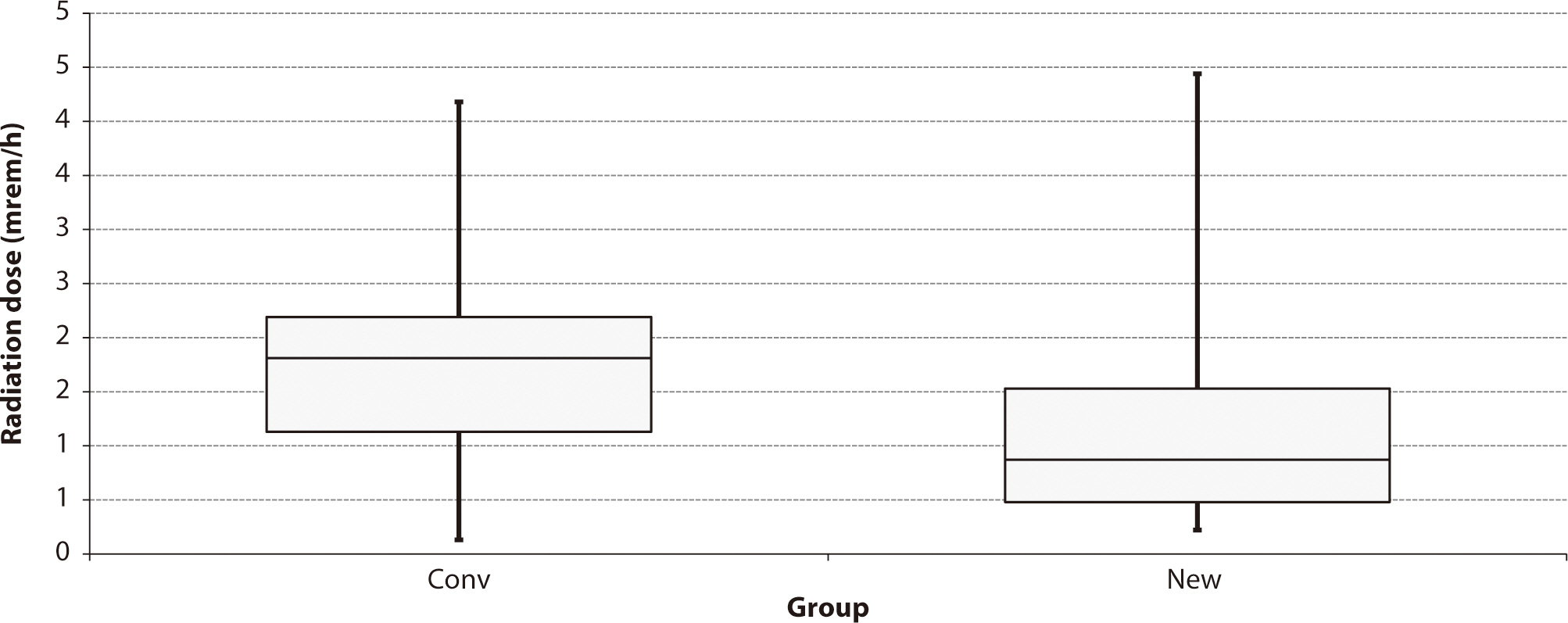
The median radiation doses to which the Sawbones were exposed were 1.81
millirem/hour for the conventional technique and 0.87 millirem/hour for the
new method. The dose received with the new technique was significantly lower
than that received with the conventional approach (Wilcoxon W=263.0,
corrected Z=−2.2150, P=0.0268,
Fig.
5).
Fig. 5.Comparison of radiation dose administered to the Sawbones between
the conventional technique (Conv) and the new method (New) for
intramedullary nailing. Values represent doses of radiation, in
millirem/hour.
Attempts required for success
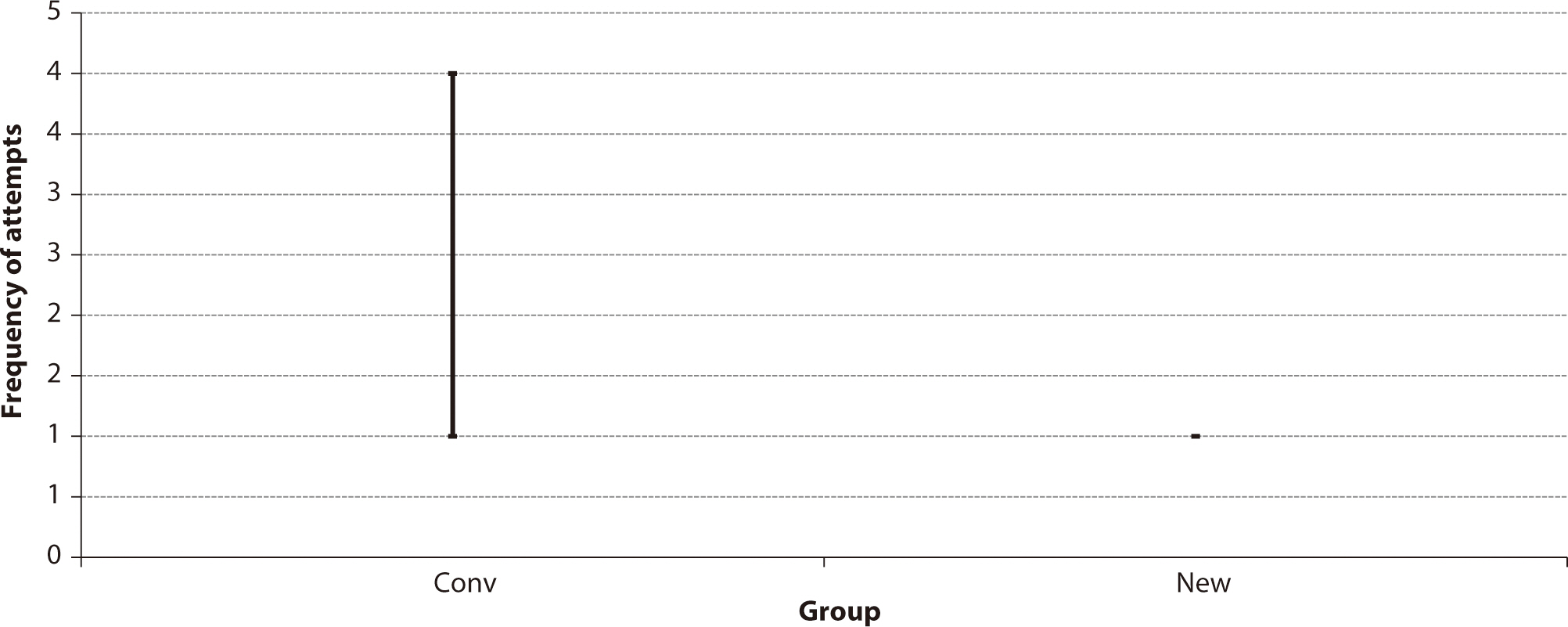
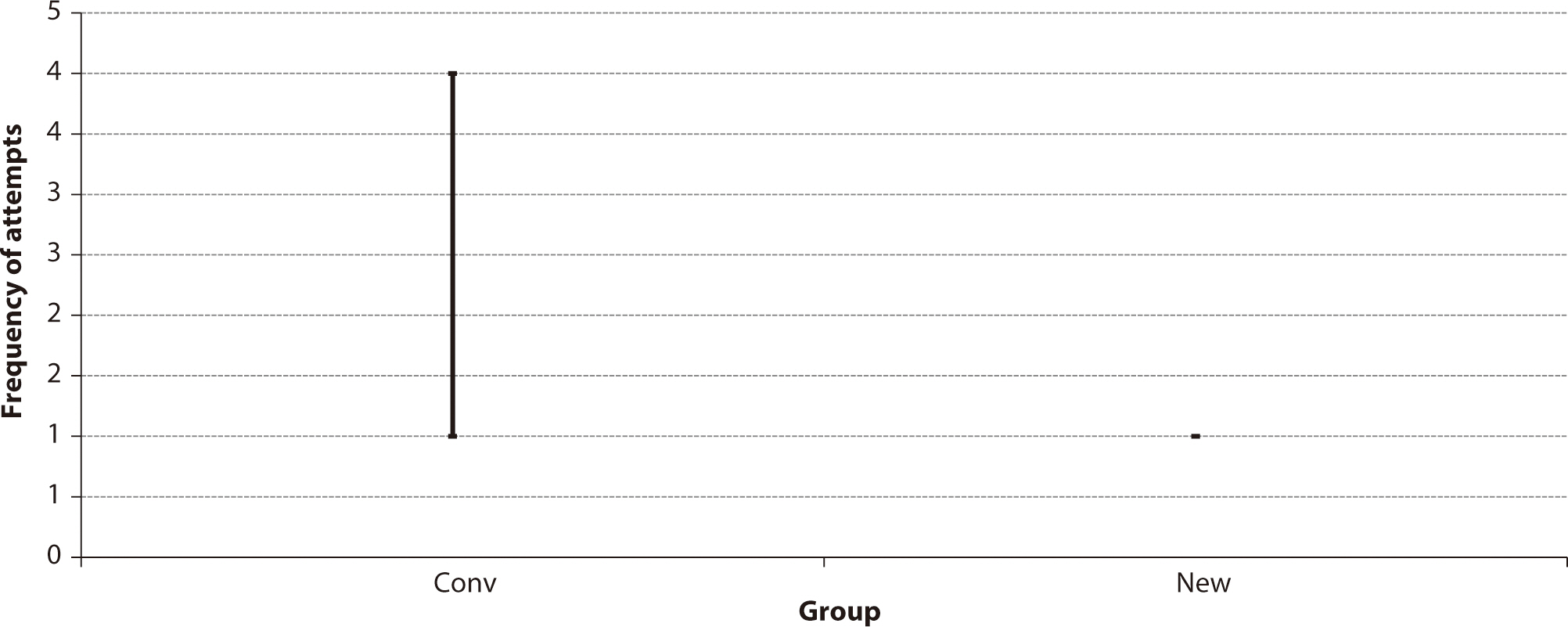
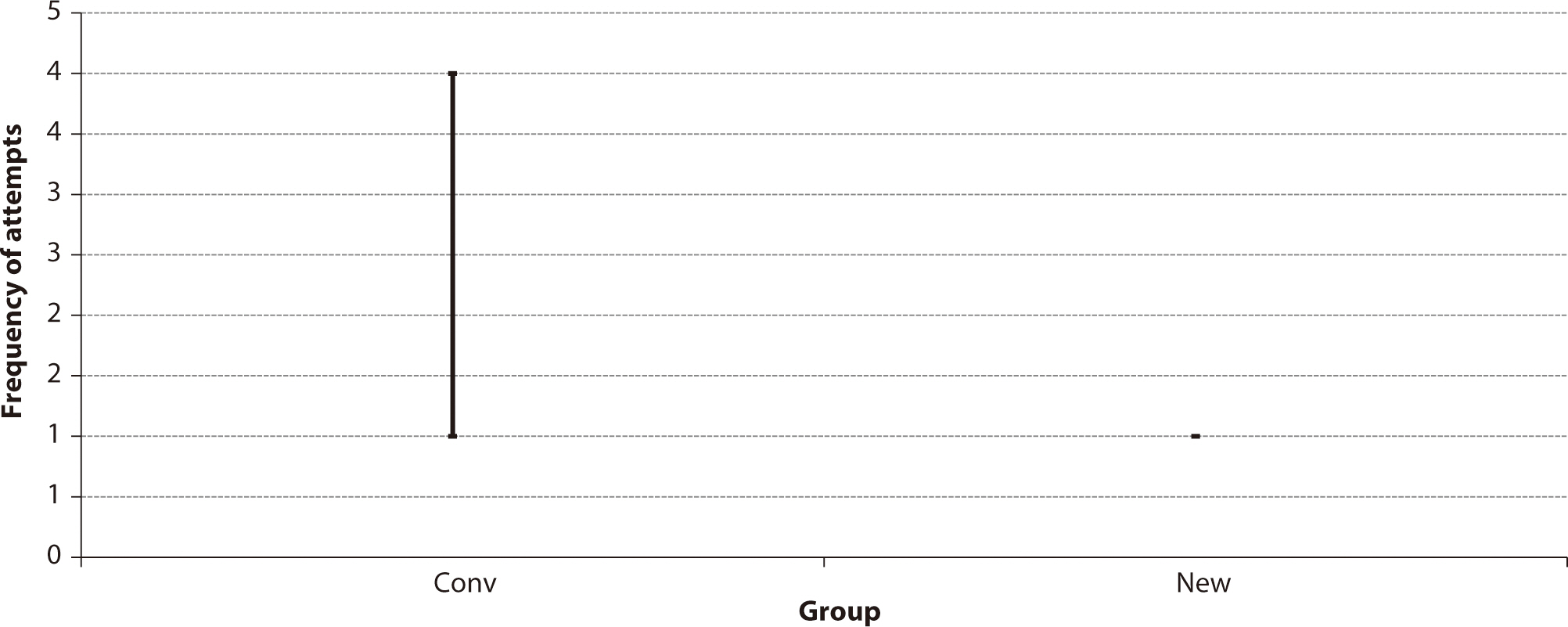
The new technique required only one attempt to succeed, whereas the
conventional technique took a maximum of four attempts (Wilcoxon W=297.0,
corrected Z=−2.0889, P=0.0367,
Fig.
6).
Fig. 6.Comparison of the frequency of attempts between the conventional
technique (Conv) and the new method (New) for intramedullary
nailing. Values represent frequencies of attempts.
Discussion
Key results
A new technique for interlocking screw insertion during IM nailing, which
utilizes a Steinmann pin and hammer, offers surgeons a time-saving approach with
lower radiation exposure and fewer attempts compared to the conventional method
not employing a Steinmann pin and hammer.
Interpretation
Two considerations are key when creating interlocking holes: the entry point and
the drilling direction. The initial and most critical step involves precisely
adjusting the C-arm to align the interlocking holes so they appear as a perfect
circle. Drilling should commence only after achieving this circle. Our technique
specifically addresses the second consideration, facilitating easy drilling. The
most difficult aspect of drilling is that if the drill bit creates an incorrect
hole, subsequent attempts to establish a correct pathway often fail because the
drill bit tends to slip into the previous hole. In our study, we trained an
inexperienced resident who then achieved a near 100% success rate, demonstrating
an acceptable learning curve for this challenging procedure. Additionally, our
technique resulted in less radiation exposure than the conventional method,
despite a longer mean operative time. However, the conventional technique
included an outlier value, indicating that once an error occurs, the procedure
can take markedly longer to complete (Dataset 1).
Our proposed technique was designed to increase the precision of drill
orientation. With the conventional method, the drill bit may not align correctly
with the intended bone path, potentially failing to penetrate the near and far
cortex holes of the nail at the appropriate angle. If the drill bit passes
through the near cortex hole and the tip abuts the far hole, repositioning the
drill bit can be challenging due to the pre-existing bone path. Should the
surgeon opt to replace the drill bit with a Steinmann pin, the pin can be gently
tapped into the far cortex hole of the nail, where it will slide into place.
Notably, a Steinmann pin could also be utilized from the outset of the
procedure.
A Steinmann pin was chosen over a drill bit for several reasons. First, a drill
bit has a smaller core diameter and is stiffer than a Steinmann pin, increasing
the risk of breakage when redirecting the bit within the bone. Second, the use
of a Steinmann pin eliminates the need for secondary drilling, as the pin
matches the drill bit in diameter. Third, unlike a drill bit, a Steinmann pin
can be driven into the bone with a hammer. Finally, the Steinmann pin’s
tip is both narrower and sharper than that of the drill bit, allowing it to gain
purchase with the bone even if the initial hole is slightly misaligned.
We opted for a hammer instead of a drill because a drill attached to a Steinmann
pin often obscures the radiologic view of the hole. Additionally, the drilling
process can cause more damage to both the Steinmann pin and the nail. In
contrast, when tapping the Steinmann pin with a hammer, the hole remains
constantly visible. This method allows the Steinmann pin to slide into the hole
without grinding against the nail. When the entry point is accurate, the success
rate of inserting a Steinmann pin is nearly 100%. Even with a slightly
inaccurate starting point, an interlocking hole can still be created using the
hammer technique. However, this may result in the oblique insertion of the
interlocking screw. Our technique appears beneficial and effective when a
substantial distance separates the near and far cortices, or when the insertion
site is located at the metaphysis rather than the diaphysis. Moreover, using a
hammer to insert the Steinmann pin can help prevent damage to the surrounding
soft tissue.
Limitations
This study had several limitations. First, the clinical procedure differs from
that performed on the Sawbones. In clinical practice, the soft tissues
surrounding the femur could impede the accuracy of initial pin placement and the
maintenance of the angle and location of the pin during drilling. Moreover,
Sawbones are easier to drill than living bones, particularly those of younger
individuals. Nevertheless, this study demonstrated significant differences
between the two techniques when performed on the same Sawbones model. We expect
these differences to be reproducible in real-world scenarios, although it may
take longer to complete the procedure with either technique. Second, the sample
size was primarily determined by the availability of resources rather than
statistical power calculations. Finally, bias is a possibility, as the resident
was aware of the technique being used. To address this concern and avoid a
ceiling effect, we ensured that the resident was thoroughly trained in both
techniques prior to the experiment to minimize any learning curve effects.
Furthermore, we randomized the order in which the techniques were applied to
each specimen to reduce the impact of systematic bias.
Generalizability
This new technique may aid in the insertion of interlocking screws during IM
nailing procedures in hospitals around the world. Several companies manufacture
instruments to support the precise placement of distal interlocking screws, such
as the Radiolucent Drive (Synthes) and the Trigen Sureshot (Smith &
Nephew, London, UK) [
8]. However, these
tools are expensive, and surgeons in underdeveloped or developing nations often
cannot afford them. Our method employs a relatively inexpensive Steinmann pin,
eliminating the need for costly equipment. Additionally, this technique is
applicable to all types of IM nailing, including that of the humerus and
tibia.
Our technique, which employs a Steinmann pin and hammer, is a reliable,
reproducible, and cost-efficient approach for the creation of distal
interlocking holes.
Authors' contributions
-
Project administration: Deslivia MF, Kim HJ, Kim SH
Conceptualization: Deslivia MF, Kim HJ, Kim SH, Lee SJ
Methodology & data curation: Deslivia MF, Kim HJ, Kim SH
Funding acquisition: not applicable
Writing - original draft: Deslivia MF, Lee SJ
Writing - review & editing: Deslivia MF, Kim HJ, Kim SH, Lee SJ
Conflict of interest
-
No potential conflict of interest relevant to this article was reported.
Funding
-
Not applicable.
Data availability
-
Data files are available from Harvard Dataverse: https://doi.org/10.7910/DVN/ND7IIK
Dataset 1. Results of the comparison between new and conventional methods in
terms of time savings, radiation dose exposure to the Sawbones, and number of
attempts
Acknowledgments
Not applicable.
Supplementary materials
-
Not applicable.
References
- 1. Wolinsky P, Tejwani N, Richmond JH, Koval KJ, Egol K, Stephen DJ. Controversies in intramedullary nailing of femoral shaft
fractures. Instr Course Lect 2002;51:291-303.
- 2. Baltov A, Mihail R, Dian E. Complications after interlocking intramedullary nailing of
humeral shaft fractures. Injury 2014;45:Suppl 1. S9-S15.
- 3. Ikpeme I, Ngim N, Udosen A, Onuba O, Enembe O, Bello S. External jig-aided intramedullary interlocking nailing of
diaphyseal fractures: experience from a tropical developing
centre. Int Orthop 2011;35(1):107-111.
- 4. Levin PE, Schoen RW Jr, Browner BD. Radiation exposure to the surgeon during closed interlocking
intramedullary nailing. J Bone Joint Surg Am 1987;69(5):761-766.
- 5. Müller LP, Suffner J, Wenda K, Mohr W, Rommens PM. Radiation exposure to the hands and the thyroid of the surgeon
during intramedullary nailing. Injury 1998;29(6):461-468.
- 6. Harrington P, Howell F. An aid to distal locking of the Russell-Taylor humeral
nail. Injury 1998;29(9):732-733.
- 7. Knudsen CJ, Grobler GP, Close RE. Inserting the distal screws in a locked femoral
nail. J Bone Joint Surg Br 1991;73(4):660-661.
- 8. MacMillan M, Gross RH. A simplified technique of distal femoral screw insertion for the
Grosse-Kempf interlocking nail. Clin Orthop Relat Res 1988;226:252-259.
- 9. Maqungo S, Horn A, Bernstein B, Keel M, Roche S. Distal interlocking screw placement in the femur: freehand versus
electromagnetic assisted technique (sureshot). J Orthop Trauma 2014;28(12):e281-e283.
- 10. Owen TD, Coorsh J. Insertion of the distal locking screws in femoral nailing: a
simplified technique. Injury 1993;24(2):101-103.
Figure & Data
Citations
Citations to this article as recorded by

- Unresolved policy on the new placement of 2,000 entrants at Korean
medical schools and this issue of Ewha Medical
Journal
Sun Huh
The Ewha Medical Journal.2024;[Epub] CrossRef