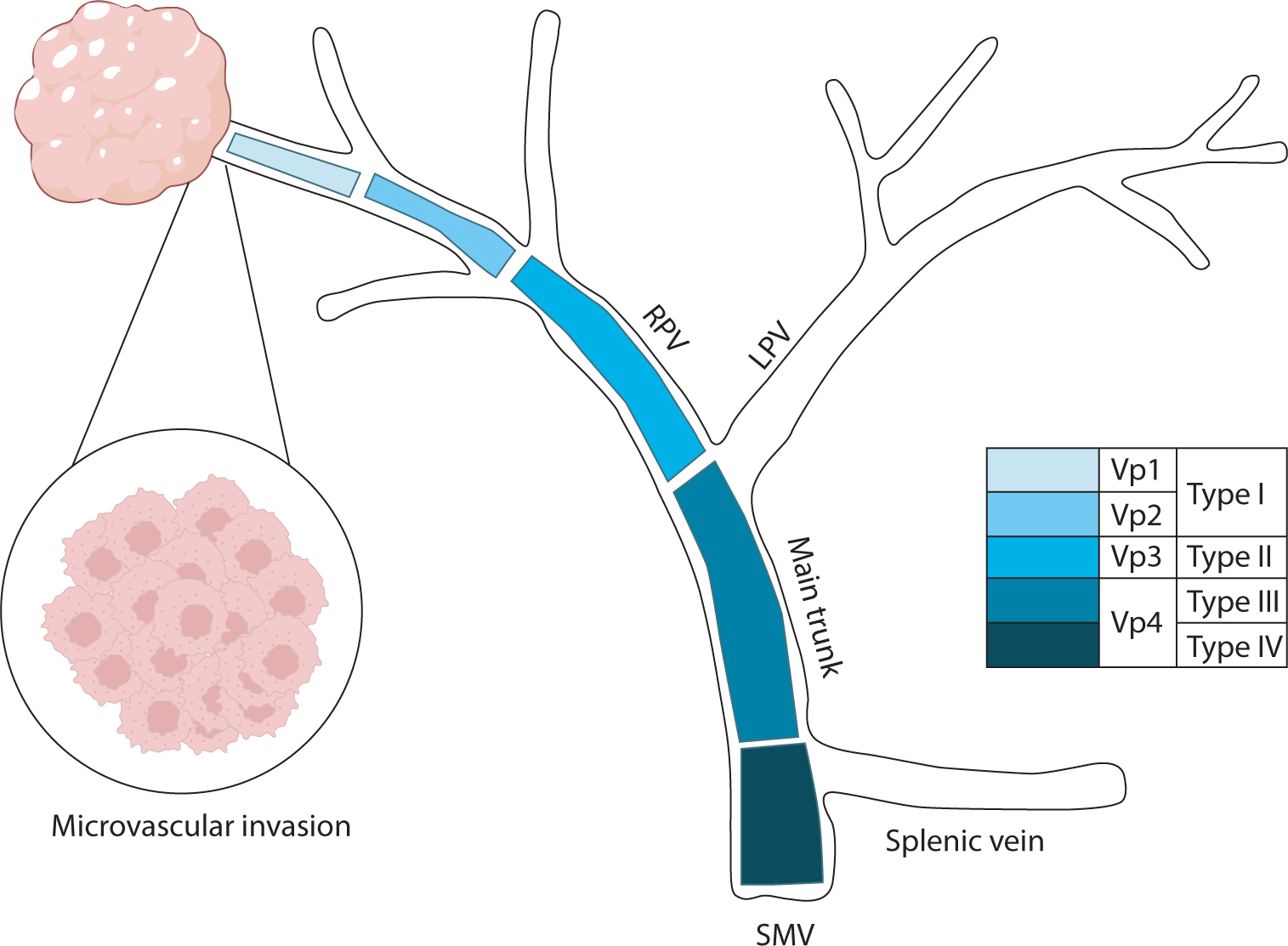
Hepatocellular carcinoma with portal vein tumor thrombosis presents a significant therapeutic challenge due to its poor prognosis and limited treatment options. This review thoroughly examines diagnostic methods, including imaging techniques and classification systems such as the Japanese Vp and Cheng’s classifications, to aid in clinical decision-making. Treatment strategies encompass liver resection and liver transplantation, particularly living donor liver transplantation after successful downstaging, which have shown potential benefits in selected cases. Locoregional therapies, including hepatic arterial infusion chemotherapy, transarterial chemoembolization, transarterial radioembolization, and external beam radiation therapy, remain vital components of treatment. Recent advancements in systemic therapies, such as sorafenib, lenvatinib, and immune checkpoint inhibitors (e.g., atezolizumab plus bevacizumab) have demonstrated improvements in overall survival and progression-free survival. These developments underscore the importance of a multidisciplinary and personalized approach to improve outcomes for patients with hepatocellular carcinoma and portal vein tumor thrombosis.

Metabolic dysfunction-associated steatohepatitis (MASH) is increasingly recognized as a leading cause of hepatocellular carcinoma (HCC), the third-leading cause of cancer mortality worldwide, driven by the global obesity epidemic. Projected to become the primary cause of HCC by 2030, MASH-HCC presents unique clinical challenges. This review examines its clinical management, including surveillance strategies and treatment advances, and discusses prospects to overcome existing challenges. MASH-HCC accounts for 10%–20% of HCC cases, particularly in Western countries, with a rising incidence due to obesity. Risk factors include cirrhosis, diabetes, obesity, alcohol, smoking, genetic polymorphisms (e.g., PNPLA3), and microbiome alterations. The pathogenesis involves fibrosis, immune dysfunction (e.g., T-cell impairment), and molecular changes. Prevention focuses on lifestyle modifications. Surveillance in patients with MASH cirrhosis is crucial but is hindered by poor ultrasound sensitivity in obese patients, necessitating alternative methods. Treatment mirrors that of other HCC types, but comorbidities and potentially reduced efficacy of immunotherapy necessitate tailored approaches. MASH is becoming the leading cause of HCC, necessitating lifestyle interventions for prevention. Improved surveillance and early detection are critical but challenging due to obesity-related factors. Treatments align with those for other HCC types, but comorbidities and potential differences in immunotherapy efficacy due to T-cell dysfunction require careful consideration. Key needs include identifying molecular drivers in non-cirrhotic metabolic dysfunction-associated steatotic liver disease, developing preventive therapies, refining surveillance methods, and tailoring treatments. Trials should specifically report MASH-HCC outcomes to enable personalized therapies. Further research is needed to understand T-cell dysfunction, optimize immunotherapies, and identify predictive biomarkers.
 , Jeong-Ju Yoo
, Jeong-Ju Yoo , Sang Gyune Kim
, Sang Gyune Kim , Young Seok Kim
, Young Seok Kim
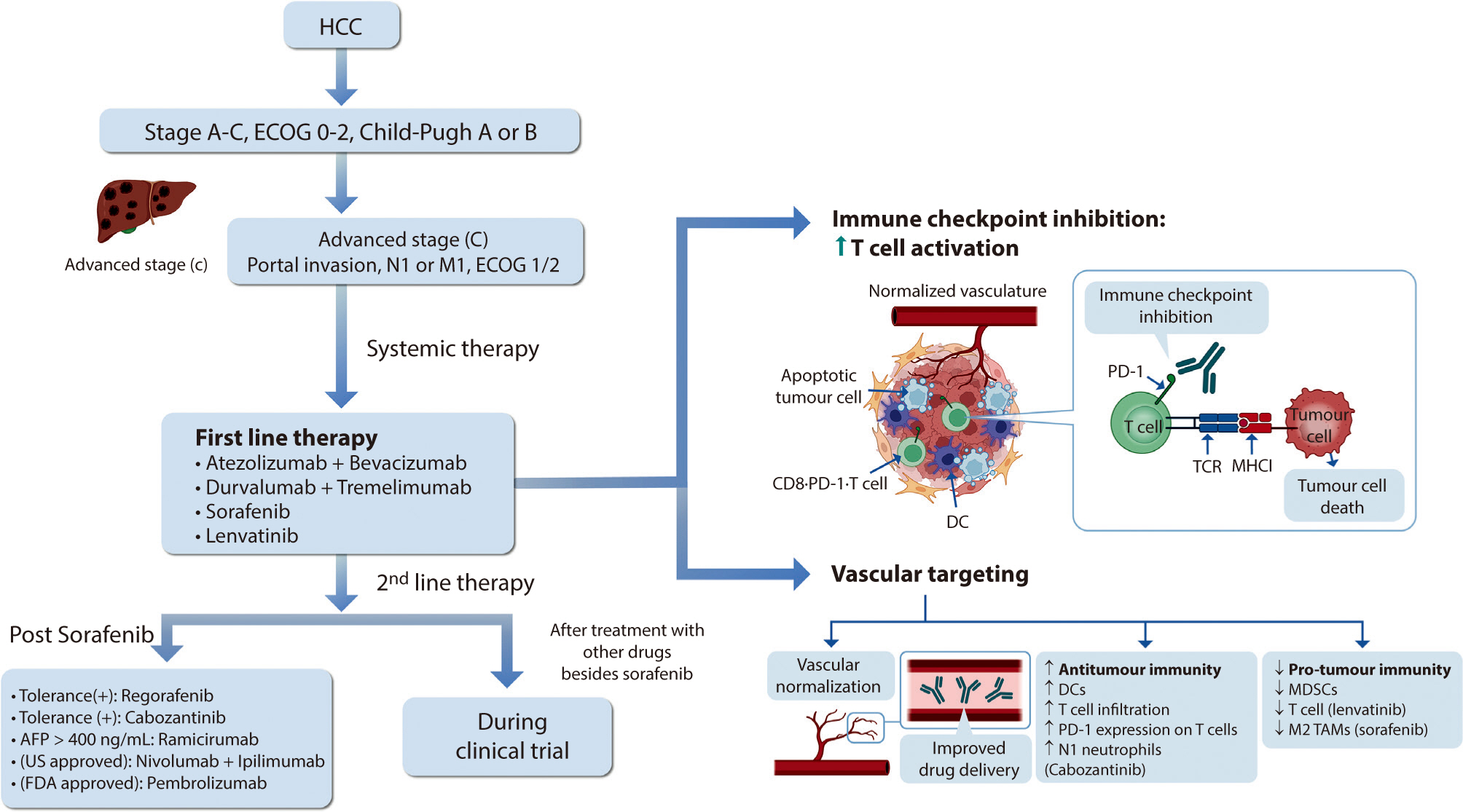
Hepatocellular carcinoma (HCC) remains a critical health concern in Korea, ranking as the second leading cause of cancer mortality and imposing substantial economic burdens, particularly among the working-age population. This review examines recent advancements in treating advanced HCC, referencing the updated 2022 HCC guidelines and the Barcelona Clinical Liver Cancer system. Historically, first-line systemic therapies included sorafenib and lenvatinib, with regorafenib, cabozantinib, or ramucirumab serving as second-line options. Since 2020, immune checkpoint inhibitors have shown superior overall survival than sorafenib, leading to the adoption of combination therapies such as atezolizumab with bevacizumab and durvalumab with tremelimumab as first-line treatments. The IMbrave150 study demonstrated that atezolizumab–bevacizumab significantly extended median overall survival and progression-free survival, with the longest survival reported in any phase 3 trial for advanced HCC. Similarly, the HIMALAYA study indicated that durvalumab combined with tremelimumab significantly improved survival rates. Second-line therapies now include regorafenib, cabozantinib, ramucirumab, nivolumab with ipilimumab, and pembrolizumab, each offering benefits for specific patient populations. Nonetheless, these therapies are associated with side effects that require careful management. Traditional targeted therapies can lead to hypertension, cardiovascular events, and hand-foot skin reactions, whereas immune checkpoint inhibitors may cause immune-related adverse events affecting the skin, gastrointestinal tract, and endocrine system. Clinicians must be well-versed in these treatments and their potential side effects to provide optimal patient care. The emergence of combination therapies targeting complex biological pathways signifies a new paradigm in HCC treatment, emphasizing the importance of continuous education and vigilant monitoring to optimize patient outcomes.
Citations

 , Won Kim
, Won Kim
Understanding the effects of sex and sex differences on liver health and disease is crucial for individualized healthcare and informed decision-making for patients with liver disease. The impact of sex on liver disease varies according to its etiology. Women have a lower prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD) than men. However, postmenopausal women face a higher risk of advanced liver fibrosis due to hormonal influences. Sex differences affect the pathogenesis of MASLD, which involves a complex process involving several factors such as hormones, obesity, and the gut microbiome. Furthermore, sex-related differences in the development of MASLDrelated hepatocellular carcinoma have been observed. The sex-specific characteristics of MASLD necessitate an individualized management approach based on scientific evidence. However, research in this area has been lacking. This article reviews the current understanding of sex differences in MASLD.
Citations

 , Min Jeong Kim
, Min Jeong Kim , Seung Yon Baek
, Seung Yon Baek
To evaluate MRI findings of non-recurrent hepatocellular carcinomas with lipiodol uptake (LHCCs) treated with transarterial chemoembolization.
28 LHCCs were divided into two groups according to amount of lipiodol uptake and tumor size, retrospectively. According to amount of lipiodol uptake, HCCs were classified into group A with dense lipiodol uptake (more than 90%) and group B with partial lipiodol uptake (between 50% and 90%). For HCC size analysis, group I was defined by a longest diameter of less than 2 cm, and group II was defined by a longest diameter of greater than or equal to 2 cm.
In group A (n=16), eight LHCCs showed high signal intensity (SI) on T2-weighted images (T2WI), ten LHCCs showed low SI on T1-weighted imaged (T1WI), six LHCCs showed decreased SI at higher b value of diffusion-weighted images (DWI). In group B (n=12), six LHCCs revealed high SI on T2WI, six LHCCs revealed low SI on T1WI, ten LHCCs decreased SI at higher b value of DWI. As compared with tumor size and SI, six of 12 LHCCs in group I and eight of 16 LHCCs in group II showed high SI on T2WI. Six LHCCs in group I and ten LHCCs in group II showed low SI on T1WI. All LHCCs were not enhanced.
Signal intensities of LHCCs were variable, but more than half of LHCCs showed high SI on T2WI, low SI on T1WI, decreased SI at higher
Citations

 , Joo Ho Lee
, Joo Ho Lee , Yun Bin Lee
, Yun Bin Lee , Hana Park
, Hana Park , Seong Gyu Hwang
, Seong Gyu Hwang , Kyu Sung Rim
, Kyu Sung Rim
Acute clinical deterioration in patients with chronic liver disease is called acute on chronic liver failure (ACLF). Principles of management of ACLF consist of early identifying etiology of liver disease, rapid intervention of precipitating event and discreet intensive cares. Despite medical intensive cares, if liver failure progresses, liver transplantation could be the other option. Also, liver transplantation is the only treatment that offers a chance of cure for hepatocellular carcinoma (HCC) and the underlying liver cirrhosis simultaneously. Emergent living donor liver transplantation (LDLT) can be performed for patients with acute liver failure and improves survival rate, especially in circumstances which liver graft is often not available because of deceased donors are not affordable. Here, we describe a chronic hepatitis B patient who developed ACLF accompanying early HCC. Because he did not improved with medical care, he received emergent LDLT. After LDLT, he showed great improvement without critical complications.
Citations

 , Jeong-Mi Lee
, Jeong-Mi Lee , Ja Yoon Choi
, Ja Yoon Choi , Dong-Hoon Lew
, Dong-Hoon Lew , Ra Ri Cha
, Ra Ri Cha , Hye Won Oh
, Hye Won Oh , Hong-Jun Kim
, Hong-Jun Kim , Hyun Ju Min
, Hyun Ju Min , Hyun Jin Kim
, Hyun Jin Kim , Woon-Tae Jung
, Woon-Tae Jung , Ok-Jae Lee
, Ok-Jae Lee , Chang Yoon Ha
, Chang Yoon Ha , Sun Young Yi
, Sun Young Yi
Transcatheter arterial chemoembolization (TACE) has become an effective alternative treatment strategy for patients with inoperable hepatocellular carcinoma (HCC). Although TACE is relatively safe, acute respiratory distress syndrome associated with pulmonary lipiodol embolism is a rare and potentially fatal complication. We report a rare case of acute respiratory distress syndrome after TACE for inoperable HCC. A 75-year-old man, with huge HCC in right lobe, was treated by TACE for the first time. Seven hours after uneventful TACE procedure, he felt dyspneic and his oxygen saturation recorded by pulse oximetry (SpO2) fell to 80% despite of applying non-rebreathing mask. He underwent mechanical ventilation with a protective ventilatory strategy. We experienced a case of acute respiratory distress syndrome after TACE for HCC.
 , Yoo-Ri Kim
, Yoo-Ri Kim , Hyun-Mi Heo
, Hyun-Mi Heo , Suh-Eun Bae
, Suh-Eun Bae , Myung-Won Lee
, Myung-Won Lee , Yun-Jung Choi
, Yun-Jung Choi , Go-Heun Kim
, Go-Heun Kim , Tae-Hun Kim
, Tae-Hun Kim , Kwon Yoo
, Kwon Yoo , Il-Hwan Moon
, Il-Hwan Moon
Hepatocellular carcinoma(HCC)is one of common causes of cancer-related death in Korea where the majority of HCC patients were Hepaitc B virus(HBV)carriers and have cirrhosis. Transarterial chemoembolization(TACE)is commonly applied to the treatment of multinodular HCC in Korea and careful selection of candidate is important for the risk of various side effects. Besides common side effects as fever, nausea, abdominal pain and elevation of liver enzyme, TACE may predispose to hepatic failure, ischemic cholecystitis, pulmonary embolism, cerebral embolism and pneumonitis. In previous studies, some cases of pulmonary and cerebral embolism cases were reported but lipiodol pneumonitis after TACE was rarely reported. A 65-year-old woman with a multinodular HCC associated with HBV infection, was treated with TACE. Seven days after the procedure, nonspecific respiratory symptoms such as dyspnea and dry cough developed. Chest X-ray and chest computed tomography showed diffuse ground glass opacities in whole lung fields, suggestive of lipiodol pneumonitis. After several days of supportive care with steroid administration, radiologic abnormalities and subjective symptoms were much improved, considered that the disease was compatible with lipiodol pneumonitis.
Citations


