 , Hyun Kang
, Hyun Kang
 , Oh Haeng Lee
, Oh Haeng Lee , Hyun Kang
, Hyun Kang
Citations

 , Minsung Kim
, Minsung Kim
Enhanced recovery after surgery (ERAS) protocols are designed to minimize surgical stress, preserve physiological function, and expedite recovery through standardized perioperative care for primary colorectal surgery patients. This narrative review explores the benefits of current ERAS protocols in improving outcomes for these patients and provides insights into future advancements. Numerous studies have shown that ERAS protocols significantly reduce the length of hospital stays by several days compared to conventional care. Additionally, the implementation of ERAS is linked to a reduction in postoperative complications, including lower incidences of surgical site infections, anastomotic leaks, and postoperative ileus. Patients adhering to ERAS protocols also benefit from quicker gastrointestinal recovery, marked by an earlier return of bowel function. Some research indicates that colorectal cancer patients undergoing surgery with ERAS protocols may experience improved overall survival rates. High compliance with ERAS protocols leads to better outcomes, yet achieving full adherence continues to be a challenge. Despite these advantages, implementation challenges persist, with compliance rates affected by varying clinical practices and resource availability. However, the future of ERAS looks promising with the incorporation of prehabilitation strategies and technologies such as wearable devices and telemedicine. These innovations provide real-time monitoring, enhance patient engagement, and improve postoperative follow-up, potentially transforming perioperative care in colorectal surgery and offering new avenues for enhanced patient outcomes.
Citations

 , Ryung-Ah Lee
, Ryung-Ah Lee
The capabilities of artificial intelligence (AI) have recently surged, largely due to advancements in deep learning inspired by the structure and function of the neural networks of the human brain. In the medical field, the impact of AI spans from diagnostics and treatment recommendations to patient engagement and monitoring, considerably improving efficiency and outcomes. The clinical integration of AI has also been examined in specialties, including pathology, radiology, and oncology. General surgery primarily involves manual manipulation and includes preoperative, intraoperative, and postoperative care, all of which are critical for saving lives. Other fields have strived to utilize and adopt AI; nonetheless, general surgery appears to have retrogressed. In this review, we analyzed the published research, to understand how the application of AI in general surgery differs from that in other medical fields. Based on previous research in other fields, the application of AI in the preoperative stage is nearing feasibility. Ongoing research efforts aim to utilize AI to improve and predict operative outcomes, enhance performance, and improve patient care. However, the use of AI in the operating room remains significantly understudied. Moreover, ethical responsibilities are associated with such research, necessitating extensive work to gather evidence. By fostering interdisciplinary collaboration and leveraging lessons from AI success stories in other fields, AI tools could be specifically tailored for general surgery. Surgeons should be prepared for the integration of AI into clinical practice to achieve better outcomes; therefore, the time has come to consider ethical and legal implications.
Citations


Anastomotic leakage (AL) after colorectal surgery is a significant concern, as it can lead to adverse functional and oncologic outcomes. Numerous studies have been conducted with the aim of identifying risk factors for AL and developing strategies to prevent its occurrence, thereby reducing the severe morbidity associated with AL. The intraoperative method for reducing AL includes a mechanical assessment of AL, an assessment of bowel perfusion, drain placement, and the creation of diverting stomas. The anastomosis technique is also associated with AL, and the appropriate selection and accurate application of anastomotic methods are crucial for preventing AL. Indocyanine green fluorescence imaging has recently gained popularity as a method for assessing bowel perfusion. While it is useful for detecting bowel perfusion, standardized protocols and measurement methods need to be established to ensure its reliability and effectiveness in clinical practice. The use of intraoperative drains to reduce AL has produced inconsistent results, and the routine adoption of this practice is not currently recommended. Diverting stomas can be used to help reduce the morbidity associated with AL. However, it is important to carefully consider the complications that can arise directly from the stoma itself. It should be noted that while a stoma can reduce AL, it cannot completely prevent it. This descriptive review examines various intraoperative methods aimed at reducing AL, discussing their effectiveness in reducing AL.
Citations

Over the past 3 years, the COVID-19 pandemic has posed significant challenges to the healthcare system, leading to delays in the diagnosis and treatment of various diseases due to the need for social distancing measures. Colorectal cancer has not been immune to these disruptions, and research in various countries has explored the impact of COVID-19 on the diagnosis and treatment of colorectal cancer. One notable consequence has been the postponement of colorectal cancer screenings, potentially resulting in disease progression, which can adversely affect surgical and oncological outcomes. Furthermore, the treatment approach for colorectal cancer may vary depending on the extent of disease progression and the healthcare policies implemented in response to the COVID-19 pandemic. In this systematic review, we examine treatment strategies, surgical outcomes, and oncological variables across multiple studies focusing on colorectal cancer treatment during the COVID-19 pandemic. The purpose of this analysis was to assess how medical policies enacted in response to the COVID-19 pandemic have influenced the outcomes of colorectal cancer treatment. We hope that this review will provide valuable insights and serve as a foundational resource for developing guidelines to address potential medical crises in the future.

The primary objective in the treatment of early rectal cancer is to achieve optimal oncological control while minimizing the long-term impact of therapeutic interventions on patients' quality of life. The current standard of care for most stage I and II rectal cancers involves radical surgery, specifically total mesorectal excision. Although total mesorectal excision is generally curative for early rectal cancers, it can significantly affect patients' quality of life by potentially necessitating a permanent colostomy and causing bowel, bladder, and sexual dysfunction. Given the morbidity associated with radical surgery, alternative approaches to managing early rectal cancer, such as local excision through transanal excision, transanal endoscopic microsurgery, and transanal minimally invasive surgery, have been investigated. If these surgical approaches are applied cautiously to carefully selected cases of early rectal cancer, it is anticipated that these local procedures will achieve comparable oncological outcomes to the established standard of radical surgery, potentially offering superior results regarding morbidity, mortality, and overall quality of life.

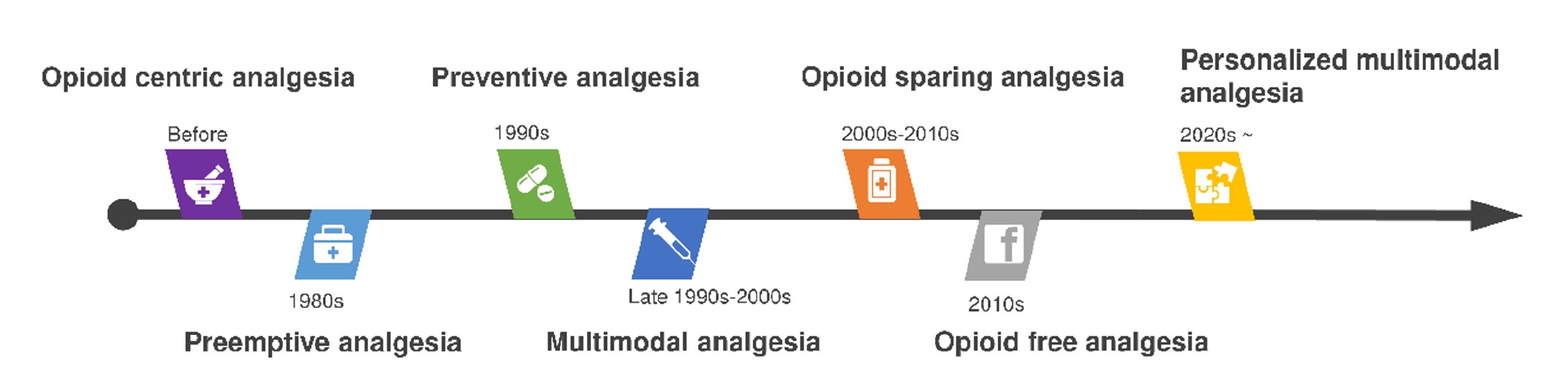
Enhanced recovery after surgery (ERAS) aims to promote postoperative recovery in patients by minimizing the surgical stress response through evidence-based multimodal interventions. In 2023, updated clinical practice guidelines were published in North America, potentially superseding the most recent guidelines previously announced at the ERAS Society in 2019. This review compares and reviews these two guidelines to examine the principle of ERAS and items related to colorectal surgery and to introduce the latest relevant study results published within the last 5 years. In the pre-hospitalization stage, the concept of pre-hospitalization is emphasized; this involves checking and reinforcing the patient’s nutritional status and physical functional status before surgery. In the preoperative stage, large-scale studies have prompted a change in the recommendation of mechanical bowel preparation combined with oral antibiotics in elective colorectal surgery. In the intraoperative stage, laparoscopic surgery has become a widespread and important component of ERAS, and more technologically advanced single-incision laparoscopic surgery and robotic surgery are the focus of active research. Ileus-prevention items, such as opioid-sparing multimodal pain management and euvolemic fluid therapy, are recommended in the postoperative stage. The adoption of ERAS protocols is expanding to encompass a wide range of surgical procedures, clinical scenarios, healthcare institutions, and professional medical societies. In order to maximize the effect by increasing adherence to ERAS, medical staff must fully understand the clinical basis and meaning of each item, and the protocol must be maintained and developed steadily through a team approach and audit system.
Citations


Fecal incontinence (FI) is recurrent uncontrolled passage of fecal material in patients. The life expectancy of humans has increased. Elderly patients have a significant rate of FI. Therefore, the number of patients with FI will increase. For diagnosis of FI, the digital rectal exam, ultrasonography, and anal manometry are used. In addition, the severity of FI can be assessed using the FI score system by examining symptoms. Recent applications include three-dimensional ultrasonography and other novel approaches. The treatments for FI include biofeedback therapy, anal implant, artificial sphincter, nerve modulation, SECCA, stem cell therapy, and surgical intervention. Biofeedback therapy is a noninvasive procedure. Anal implant, stem cell therapy, and SECCA are all minimally invasive treatments. And more methods constitute intrusive treatment. None of these therapies has been conclusively demonstrated to be superior. Depending on the severity of the symptoms, a non-invasive approach or an intrusive treatment is most frequently employed. In this review, I will discuss the diagnosis and treatment options for FI.
Citations

Brain metastases are a leading cause of morbidity and mortality for patients with systemic cancer and are among the most common intracranial tumors in adults. Its incidence increases as cancer therapies improve, and patients live longer, providing new challenges to the multidisciplinary teams that manage these patients. The contemporary neurosurgical treatment of intracranial metastases has become gradually more complex as the available therapeutic options increase. For the past 50 years, whole brain radiotherapy and systemic corticosteroids have been considered as the standard of care for patients with brain metastases. However, in recent years, stereotactic radiosurgery is spotlighted as an alternative therapeutic modality for these patients because of its relatively short, convenient, and non-invasive treatment course. Stereotactic radiosurgery is a radiation therapy technique in which multiple focused radiation beams intersect over a target, which results in the delivery of highly conformal, high-dose of radiation to the target and minimal radiation to surrounding normal parenchyma. The purpose of this review is to provide an overview of stereotactic radiosurgery as a treatment modality for patients with brain metastases.
Citations

 , Hyungju Kwon
, Hyungju Kwon , Woosung Lim
, Woosung Lim , Byung-In Moon
, Byung-In Moon , Nam Sun Paik
, Nam Sun Paik
Active surveillance (AS) of papillary thyroid microcarcinoma was first suggested by Dr. Akira Miyauchi at Kuma Hospital in 1993. Based on several subsequent evidences, AS was approved by the American Thyroid Association in 2015. AS is no longer an experimental treatment but has become an acceptable standard of care for patients with low-risk thyroid cancers. No molecular markers, such as BRAF mutations, have been identified to predict the prognosis of papillary thyroid cancer. However, future molecular studies may reveal the relationship between genetic mutations and thyroid cancer prognosis. AS involves closely monitoring thyroid cancer over time, instead of immediately treating it with surgery. Patients and medical doctors should consider these two options: observation or surgery.
With advances in medicine and technology, treatment modalities for diseases have evolved. Consequently, physicians’ roles have also changed. Because of advances in endovascular treatment, neurosurgeons specializing in cerebrovascular surgery are increasingly using endovascular techniques. Accordingly, the number of so-called “hybrid neurosurgeons” who perform both traditional craniotomy cerebrovascular surgeries and endovascular treatments is on the rise. This phenomenon is also occurring in department of neurology, traditionally a non-surgical specialty, and the number of neurologists using endovascular treatments is also increasing. Nowadays endovascular treatments become more common across medical specialties such as neurointerveional radiology, neurosurgery, and neurology. In this time, what should be the role of neurosurgeons? Standardized hybrid surgeons should contribute to society by treating hemorrhagic stroke and ischemic stroke, maintaining a proper number of hybrid-neurosurgeons to ensure demand for such treatments is met. Further, more neurosurgeons should be trained to perform sophisticated traditional surgeries, as these surgeries cannot be performed by anyone else. Finally, neurosurgery patients often require a combination of surgical and medical treatment. In these situations, primary and secondary prevention are also crucial. And, many neurosurgery patients also have psychoneurotic symptoms. Within neurosurgery backgrounds, we, neurosurgeons, need to be intensivists for critical care medicine, hospitalization experts, epidemiologists, neuropsychiatry experts, and basic researchers. Because we have to be in charge of neurosurgical patients with various problems in our healthcare environment. Therefore, advancing beyond hybrid neurosurgeons and beginning an era of convergence neurosurgeons should be our role in the future.
 , Jun Seop Lee
, Jun Seop Lee , Jong Hak Kim
, Jong Hak Kim , Youn Jin Kim
, Youn Jin Kim , Jae Hee Woo
, Jae Hee Woo , Dong Yeon Kim
, Dong Yeon Kim , Jeong Jeong
, Jeong Jeong
The phase of the menstrual cycle was demonstrated to have an influence on the incidence of postoperative nausea and vomiting (PONV) after gynecologic laparoscopic surgery, but little was known for breast surgery, which was shown to have relatively higher incidence of PONV, >60%. We performed this study to investigate the influence of the phase of menstrual cycle on PONV after breast cancer surgery.
A total of 103 patients, who were scheduled for breast cancer surgery under general anesthesia, were recruited, and patients with irregular menstrual cycles, history of previous history of PONV were excluded. Groups were divided in two ways as follows: 1) gynecologic classification: premenstrual and menstrual (days 25 to 6), follicular (days 8 to 12), ovulation (days 13 to 15), and luteal phase (days 20 to 24); 2) menstrual classification: menstrual (days 1 to 8) and non-menstrual (days 9 to 28). PONV were recorded using Rhodes index of nausea, vomiting and retching at postoperative 6 and 24 hours.
The overall incidence of PONV during postoperative 24 hours was 35.4%. At the menstrual classification, the incidence of PONV at postoperative 24 hours was higher in the menstrual group than that in the non-menstrual group (16.7% vs. 4.2%, P=0.057). The severity of PONV, measured with Rhodes index of nausea, vomiting and retching was significantly different between menstrual and non-menstrual groups (P=0.034).
The duration and severity of the PONV after breast cancer surgery were demonstrated to be prolonged and aggravated during menstruation, respectively. Therefore, consideration of menstrual cycle for scheduling breast cancer surgery could effectively prevent the PONV and reduce medical cost.
Citations

 , Sung Min Chung
, Sung Min Chung , Myoung Sil Ju
, Myoung Sil Ju
The surgical modalities for treatment of chronic maxillary sinusitis have changed in recent years. The radical Caldwell-Luc operation has been replaced by the more conservative endoscopic sinus surgery(ESS). Good clinical results for the ESS technique have been reported(Wigand, 1978 ; Stammberger, 1991 ; Kennedy, 1992), but only a few papers give detailed data on the symptoms(Kamel, 1989 ; Levin, 1990 ; Lund, 1991). From April 1992 to January 1996, a total of 118 patients(primary ESS 62 patients and ESS after previous nasal surgery 56 patients) who underwent ESS at the department of otolaryngology, Ewha womans university Hospital, were evaluated.
Preoperative nasal symptoms, except for nasal discharge were higher in revision cases. The previous most common nasal surgery was polypectomy accounting for 25(44.6%) of the 56 revision cases. All had preoperative CT scans of the ostiomeatal unit area(OMU CT) and severity of inflammatory disease had been graded by CT. In revision cases, 30(53.6%)cases had complete opacification of one or more major sinuses. But in primary ESS cases, 19(30.6%) had findings limited to the osteomeatal complex. Overall, 43(76.8%) patients benefited from ESS in revieion cases, and 58(93.5%) in primary ESS cases. Synechia was the most common complication in revision and primary FESS cases. The difference of outcomes between primary ESS and ESS after previous nasal surgery is explained by the difference of preoperative state of the sinus mucosa.
The author's review of 118 patients showed that there was significant difference in the postoperartive success rate between the primary ESS and ESS after previous nasal surgery.
 , Chong-Nahm Kim
, Chong-Nahm Kim , Soon-Kwan Hong
, Soon-Kwan Hong , Ji-Ae Lee
, Ji-Ae Lee , Ok-Kyung Chung
, Ok-Kyung Chung , Moon-Jung Kim
, Moon-Jung Kim
Rhinocerebral mucormycosis is a well-described fulminant fungal infection that typically presents in a rapidly fulminant manner. This condition is more likely to occur among patient with diabetes mellitus, malignant tumors, who have long-term steroid treatment, or who suffer from some debilitating diseases.
We report 3 cases of rhinoorbitocerebral mucormycosis, all suffered from diabetes mellitus. In all 3 cases, endoscopic sinus surgery was done and the antifungal agent(amphotericin B) was administered intravenously, and two patients died. One survivor who had focal extension of paranasal sinus and orbit, required one surgical intervention without orbital exenteration and he is alive without recurrence disease.
The severity of the disease is probably dependent upon the gost resistance to the invasion of phycomycetes. Early diagnosis and immediate, effective treatment are the key for cure of the disease.
 , Jun Hyeok Song
, Jun Hyeok Song , Kyu Man Shin
, Kyu Man Shin
Cysticercosis is the most frequent parasitosis of the central nervous system. Often medical treatment does not influence on ventricular or cisternal cysts or doesn't prevent the occurence of complications, such as hydrocephalus. So a considerable group of patients require surgical procedures, especially in cases of neural compression or intracranial hypertension or epilepsy. Recently stereotactic endoscopic removal of intraaxial small lesions using a stereotactic guiding tube and a fine endoscope was reported. We tried to control the symptomatic neurocy-sticercosis using the stereotatic endoscopic system.
We operated 4 cases of neurocysticercosis. Cerebrospinal fluid(CSF)analysis, enhanced com-puterized tomogram(CT) and magnetic resonance image(MRI) scan were performed. There were no specific findings in CSF analysis. CT and MRI scan showed single intraparenchymal lesion in 2 cases, one was cystic and the other was solid, multiple intraventricular cysts with obstructive hydrocephalus in 1 case and mixed type in 1 case. Seizures occured in all patients, partial sensory type in 3 cases who had reciprocal intraparenchymal lesion, generalized type in 1 case who had obstructive hydrocephalus by multple ventricular cysts.
For parenchymal lesions, we planned stereotactic open system endoscopic surgery with variable forceps, laser and suction. Cystic forms were removed successfully but in solid form additional transgyral microscopic removal was needed. In intraventricular lesions, we first placed stereotactic guiding tube via frontal burr hole, then replaced this to 14 Fr peelaway patheter. Through the peelaway catheter we inserted closed system endoscopy and removed the cysts with variable forceps and suctions. All intraparenchymal and intraventricular lesions were removed without specific complications except transient chemical meningitis in one case.
Stereotactic endoscopic surgery make it possible to operate cystic lesions without dege-neration(vesicular stage)wherever they locate.
 , Seung-Sin Lee
, Seung-Sin Lee
Obstructive sleep apnea syndrome (OSAS) is caused by repetitive upper-airway narrowing or collapse during sleep resulting in hypopneas and apneas. When a patient is diagnosed of OSAS with polysomnogram, he/she should receive upper airway evaluation to find the narrow site. The anatomic narrow site can be nasal cavity, nasopharynx, oropharynx, and/or hypopharynx. Surgical treatment for OSAS should be tailored to the anatomic narrow site. In this article, the authors describe surgical treatment options for OSAS.
 , Soo Mee Lim
, Soo Mee Lim , Myungsoo Kim
, Myungsoo Kim , Hyunsuk Suh
, Hyunsuk Suh
Radiation therapy has multiple roles in the treatment of meningioma although surgery remains the primary treatment of choice. In this retrospective study, we report the results of radiation therapy for meningioma as definitive, postoperative or salvage therapies.
Seventeen patients diagnosed with meningioma were treated with radiation therapy in our institute from May 2000 to October 2009. Radiation therapies were performed as definitive therapies in 8 patients, as postoperative therapies in 5 and as salvage therapies in 4. Nine patients received stereotactic radiosurgery (SRS), 2 patients fractionated stereotactic radiotherapy (FSRT), and 5 patients 3-dimensional conformal radiotherapy (3DCRT). Radiation dose were 12 to 20 Gy for SRS, 36 Gy in 9 fractions for FSRT and 50.4 Gy in 28 fractions for 3DCRT. Follow-up imaging study of computed tomography or magnetic resonance imaging was performed at 6 to 12 months intervals and neurologic exam was performed with an interval less than 6 months.
The median follow-up duration was 38 months (range, 12 to 85 months). Tumor progression after radiation therapy developed in one patient. The reduction of tumor volume measured on follow-up images were more than 20% in 4 patients and minimal change of tumor volume less than 20% were observed in 12 patients. Peritumoral edema developed in 4 patients and disappeared without any treatment. One patient had radiation necrosis.
Our experience is consistent with the current understanding that radiotherapy is as an effective and safe treatment modality for meningiomas when the tumor cannot be resected completely or when recurred after surgery.
 , Kyoung Tae Noh
, Kyoung Tae Noh , Boyoung Oh
, Boyoung Oh , Ryung-Ah Lee
, Ryung-Ah Lee , Soon-Sup Chung
, Soon-Sup Chung , Kwang Ho Kim
, Kwang Ho Kim
Hand-assisted laparoscopic surgery had both technical advantages of open surgery and better postoperative short-term follow-up results of laparoscopic surgery. We compared open colectomy, laparoscopic colectomy and hand-assisted laparoscopic colectomy, and tried to find the most effective operative modality.
90 patients, who were diagnosed with colorectal cancer and underwent colectomy in our institution, were categorized as 3 groups of open colectomy (OC) group, laparoscopic colectomy (LC) group and hand-assisted laparoscopic colectomy (HALC) group by the surgical modality.
In this study, ratio of male and female was 57 : 37, and mean age was 64.1 years old. LC group and HALC group showed longer operation time, shorter hospital stay after operation, lesser pain and earlier removal of closed drainage catheter than OC group. Amount of bleeding during operation, frequency of transfusion and incidence of complication showed no significant difference. In permanent pathologic results, the number of harvested lymph nodes had significant difference between OC group and other groups (P=0.030), but it was probably caused by the bias of the different distribution of the stages in each group. Overall 14 of the cases resulted in complications while there was no mortality.
Laparoscopic colectomy and hand-assisted laparoscopic colectomy showed better short-term follow-up results rather than open colectomy. And hand-assisted laparoscopic surgery could provide tactile sensation to operator, which lacked in laparoscopic surgery. Hand-assisted laparoscopic colectomy could be an alternative surgical option for colorectal cancer with these advantages.

Surgical approaches to the pituitary adenoma have undergone numerous refinements. Surgery on the pituitary adenoma is increasingly being performed through an endoscopic approach. The aim of this study is to report the results of a consecutive series of patients undergoing pituitary surgery using a pure endoscopic endonasal approach(EEA) and to evaluate the efficacy and safety of this procedure.
We reviewed 24 consecutive patients with pituitary adenoma who underwent purely endoscopic transsphenoidal resection of their lesions. The patients' clinical outcomes, including remission rates, degrees of tumor removal, and complications were evaluated.
Between September 2000 and August 2009, 76 patients with pituitary adenoma were operated on at Ewha University Mokdong Hospital. Of these, 24 patients were operated on using EEA. There were 18 nonfunctioning, 4 growth hormone-secreting, and 2 prolactin-secreting adenomas. Gross total removal was achieved in 62.5% of the cases after surgery. Visual disturbance was seen in 18 patients, which was improved in all patients. The main cause of failure of total removal was invasion to cavernous sinus. The remission results for patients with nonfunctioning adenomas was 83.3% and for functioning adenomas were 83.3%(75% for GH hormone-secreting, 100% for prolactin hormone-secreting), with no recurrence at the time of the last follow-up. Post-operative complications were present in 4(16.7%) cases. Three cases showed immediate postoperative CSF leakage, one case showed transient diabetes insipidus. There was no death related to the procedure in this series.
The endoscopic endonasal approach for resection of pituitary adenomas, provides acceptable results representing a safe alternative procedure to the microscopic approach. This less invasive method, associated with a small number of complications, provides acceptable tumor removal rates and represents an important tool for the achievement of good results in the pituitary surgery.

 , Seog Ki Min
, Seog Ki Min , Hyeon Kook Lee
, Hyeon Kook Lee , Woon Sup Han
, Woon Sup Han
The purpose of study is to compare the laparoscopic appendectomy with the open appendectomy in the clinical outcomes.
From March 2001 to June 204, a total 118 appendectomy were retrospectively reviewed. These were comprised of 57 laparoscopic appendectomy (LA), and 61 open appendectomy (OA) selected by random method among 1193 poen appendectomy cases during same period. Hospital stay, length of operation times, recovery of bowel function, postoperative complication, postoperative pain, pathologic classification were compared in both groups.
The operation times were 68.6 minutes (LA) and 51.6 minutes (OA), respectively (p=0.021). There no statistical differences in the duration of hospital stay, recovery of bowel function, complication rate, although LA group trend the shorter duration of the hospital stay, faster recovery of bowel function and low rarte of complication than OA group. The patient's satisfaction was higher in LA group than OA because of the operation wound scar.
The LA was no difference clinical outcomes except operation time as compared with OA. LA, however, may be have the merit of minimal invasive surgery and satisfaction of patient. So, LA method is attractive option for the management of appendicitis.
 , Min-Jung Kang
, Min-Jung Kang , Soyun Cho
, Soyun Cho , Kyu-Kwang Whang
, Kyu-Kwang Whang , Jeong-Hee Hahm
, Jeong-Hee Hahm
The field of dermatologic surgery has seen trementdous developments in the past few years.
Our purpose was to discuss current statistical data on the dermatologic patients treated by surgical methods at our institute.
We analyzed 2,334 cases of surgeries performed on 1,075 patients at the Department of Dermatology of Ewha Womans University Tongdaemun Hospital during a period of 5 years (1994. 1 - 1998. 12).
The results are summarized as folows:
1) Of the 2,334 cases of surgeries, 846 cases(36.2%) were chemical peelings, 650 cases(27.8%) cryosurgeries, 255 cases(10.9%) CO2, lasers, 209 cases(8.9%) dermabrasions, 113 cases(4.8%) scalpel surgeries, 61 cases(2.6%) Mohs micrographic surgeries, 50 cases(21.1%) sclerotherapy, 48 cases(2.0%) flap repair surgeries, 35 cases(1.5%) punch elevations, 15 cases(0.6%) hair transplantations, 13 cases(0.5%) epidermal grafts, and 2 cases(0.1%) autologous fat/collagen transplantations.
2) The ratio of male to female was 1 : 2.4 and the mean age of patients was 30.3 years.
3) A total of 1,354 cases of diseases were managed surgically : among them, the most frequent disease was scar(39.8%), followed by pigmentary disorders(30.8%), and benign or malignant tumors(21.2%).
4) With respect to the types of scars, acne scar was treated most frequently by chemical peeling (72.7% of 580 cases), atrophic scar by dermabrasion(37.3% of 126 cases), and hypertrophic scar (including burn scars) by cryosurgery(35.3% of 85 cases).
 , Myung-Hyun Kim
, Myung-Hyun Kim , Jun-Hyeok Song
, Jun-Hyeok Song , Sung-Hak Kim
, Sung-Hak Kim
Despite of recent advances in pharmacological treatment and improvement surgical and anesthetic techniques, subarachnoid hemorrhage(SHA) from ruptured intracranial aneurysms with poor clinical grades still carries unacceptably high morbidity and mortality rates. Recently surgery for aneurysmal SAH with poor clinical grade has increased interest.
The authors experienced 57 patients with poor clinical grade (Hunt and Hess grade IV-V) after ancurysmal SAH. Among them 25 patients were treated with immediate CSF drainage via ventriculostomy, blood pressure control, early angiography(except 3 patients) and surgery within 12 hour of admission.
The outcomes of patients were categorized using a four-tiered scale :
1) independent and working
2) impaired but independent
3) severly impaired and dependent
4) dead
The average age was 48(13-75) and the male to female ratio was 7:18 in surgical group. The average time to admission and surgery was 12 hours or less among the 25 patients. Among them 9 cases were dead, 2 cases were severly impaired and dependent, 3 cases were impaired but dependent, and 11 cases were independent and working. In this patient all cases, exception one could be ligated with a clip.
The above results suggest that the acute aggressive surgery based on appropriate selection in poor aneurysmal SAH patients can reduce of the mortality.

Recently, postoperative results of cervical spondylosis, disc herniation, tumor, and ossiication of posterior longitudinal ligament(OPLL) after anterior cervical surgeries have been improving due to new kinds of medical imaging, electrophysiological examinations, improved operative equipment, and improved surgical technique. However, occasional unsatisfactory cases needing a secondary operation remain. The author analyzed and developed strategies for multioperated cervical cases : all patients had two or more operations. From Sep. 93 to Aug. 98, 167 anterior cervical surgeries with fusions were performed in Dept. of Neurosurgery, Tong Dae Moon hospital. The author experienced 11 cases(6.6%) of failed anterior cervical surgeries and fusions : 8 men and 3 women. Initial diagnosis was 1 spondylosis, 2 cervical traumas, 3 disc herniations, and 5 cases of ossification of posterior longitudinal ligament. These multioperated cases were classified by the following cases : hardware-related complications, graft-related complications, and others. These groups were analyzed, and the resulting surgical strategies, including indications and techniques of anterior surgery, are described. The results of this study indicates that in order to reduce the need for multioperated cases, initial skillful surgical techniques and proper understanding of cervical spinal anatomy are necessary.

Surgical closure of patent ductus arterious(PDA) by lateral thoracotomy is considered as a standard therapy. But large incision, muscle cutting and chest pain are problematic. So I used two less invasive techniques : minithoracotomy and video-assisted thoracoscopic surgery. I tried to compare the results of them.
I reviewed the clinical records and operative reports of 22 children patients who were treated surgically between Jan. 19996 and Dec. 1996. Ten patients underwent Minithoracotomy(MT) and twelve patients Video-assisted thoracoscopic surgery(VATS). All of them were used tithanium clipping for closure of PDA.
Both groups were similar in age, body weight, Echocardiographically estimated size of PDA and Qp/Qs. All procedures were performed uneventfully. Operative time averaged 104±26 minutes for MT versus 96±31 minutes for VATS. Mean hospital stay was 7.2±1.7 days for MT and 4.6±1.2 days for VATS(p<0.05}. Postoperative hoarseness was occured in one patient(MT group) but was transient. There was no case with residual shunt confirmed by echocardiography.
Minithoracotomy and Video-assisted thoracoscopic surgery were as effective as lateral thoracotomy for closure of patent ductus arteriosus. Operative times were similar in two techniques but hospital stays were shorter in VATS group. Both MT and VATS techniques are effective and less invasive but I advocate VATS technique is more beneficial in terms of hospital stay and cosmetic aspect.
 , Chun Dong Kim
, Chun Dong Kim , Soon Kwan Hong
, Soon Kwan Hong
This study was performed to compare postoperative results of thyroplasty typeI and arytenoid adduction, which were recent phonosurgical procedures for the management of unilateral vocal cord paralysis.
Twenty-two cases of unilateral vocal cord paralysis with several etiologies were managed with thyroplasty typeI and/or arytenoid adduction. The subjective and MPT(maximum phonation time) improvements after those procedures were compared statistically.
The cause of paralysis were idiopathic(7 cases), thoracic lesion(6 cases) thyroidectomy(3 cases), neck mass excision(3 cases), neck trauma(2 cases) and diphtheria(case). The left side(15 cases) was paralyzed more frequently than the right(7 cases). There were significant increase(p=0.006) in MPT from 4 seconds preoperatively to 6 seconds postoperatively in thyrolasty cases, and also significant increase(p=0.014) from 5 seconds to 10.5 seconds in arytenoid adduction cases. Better result were observed in subjective improvement and MPT(p=0.0011) with arytenoid adduction. There was no significant complication.
Both arytenoid adduction and thyroplasty were effective and safe phonosurgical procedures for unilateral vocal cord paralysis. Better results were observed in arytenoid add-uction cases.

